Peripheral Artery Disease (PAD) is a common circulatory problem in which narrowed arteries reduce blood flow to your limbs. This condition can have significant impacts on your health and quality of life. Understanding PAD is crucial for early detection, effective treatment, and preventing complications. This comprehensive guide will provide essential information about PAD, including its symptoms, causes, risk factors, diagnosis, and treatment options.
Introduction
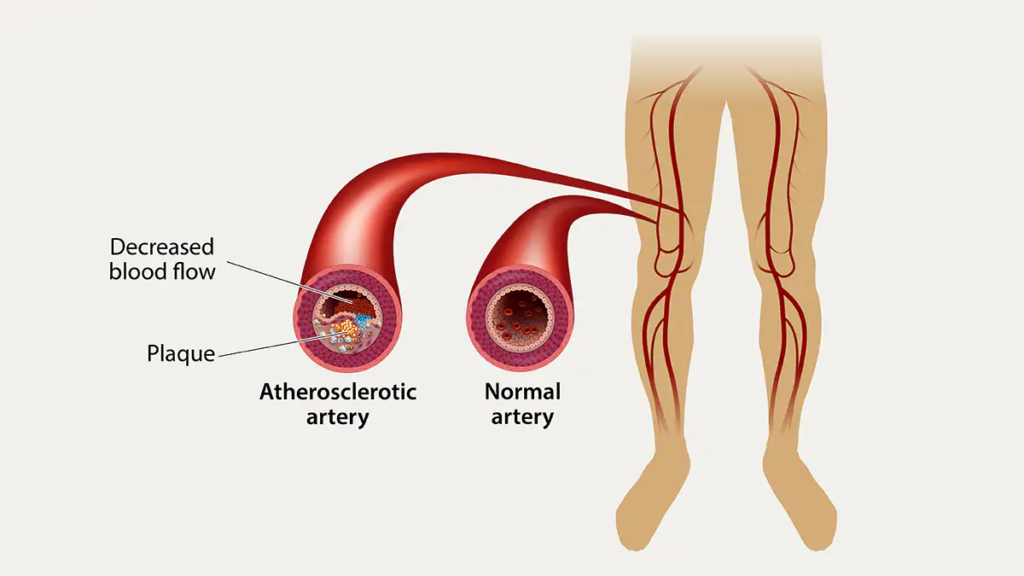
Peripheral Artery Disease (PAD) affects millions of people worldwide, particularly those over the age of 50. It’s a serious condition that often goes undiagnosed because its symptoms can be mistaken for other health issues. PAD is primarily caused by atherosclerosis, a buildup of fatty deposits in the arteries that can lead to reduced blood flow. Recognizing the signs and seeking timely medical advice can significantly improve outcomes for those affected by PAD.
Understanding Peripheral Artery Disease (PAD)
Peripheral Artery Disease (PAD) is a condition where the arteries supplying blood to the limbs, usually the legs, become narrowed or blocked due to atherosclerosis. This restriction of blood flow can lead to symptoms like leg pain while walking (claudication), numbness, and even tissue damage. PAD is a manifestation of systemic atherosclerosis, which means individuals with PAD are at higher risk of heart attack and stroke.
Causes of Peripheral Artery Disease (PAD)
The primary cause of Peripheral Artery Disease (PAD) is atherosclerosis, where plaque builds up in the walls of the arteries. This plaque is composed of fat, cholesterol, calcium, and other substances found in the blood. Over time, this plaque hardens and narrows the arteries, restricting blood flow. Other causes include blood vessel inflammation, injury to the limbs, unusual anatomy of the ligaments or muscles, and radiation exposure.
Risk Factors for Peripheral Artery Disease (PAD)
Several risk factors increase the likelihood of developing Peripheral Artery Disease (PAD), including:
- Smoking: The most significant risk factor for PAD.
- Diabetes: Increases the risk of PAD and can accelerate its progression.
- High Blood Pressure: Can damage the arteries and contribute to the development of PAD.
- High Cholesterol: Leads to plaque buildup in the arteries.
- Obesity: Extra weight increases the strain on the heart and blood vessels.
- Age: The risk of PAD increases with age, particularly after 50.
- Family History: A family history of PAD, heart disease, or stroke can increase your risk.
- Sedentary Lifestyle: Lack of physical activity contributes to obesity and poor circulation.
Symptoms of Peripheral Artery Disease (PAD)
Peripheral Artery Disease (PAD) symptoms can vary, and some individuals may not experience any symptoms, especially in the early stages. Common symptoms include:
- Claudication: Pain or cramping in the legs or arms that occurs with activity and subsides with rest.
- Leg Numbness or Weakness: Reduced blood flow can cause numbness or weakness in the legs.
- Coldness in Lower Leg or Foot: Compared to the other leg or foot.
- Sores on Toes, Feet, or Legs: That won’t heal.
- Change in Leg Color: Shiny skin on the legs.
- Hair Loss or Slower Hair Growth: On the feet and legs.
- Slower Growth of Toenails.
- No Pulse or Weak Pulse: In the legs or feet.
- Erectile Dysfunction: In men, especially those with diabetes.
Diagnosis of Peripheral Artery Disease (PAD)
Early diagnosis of Peripheral Artery Disease (PAD) is crucial for preventing complications. The diagnostic process includes:
- Medical History and Physical Exam: The doctor will review your symptoms and medical history and perform a physical exam.
- Ankle-Brachial Index (ABI): A common test that compares the blood pressure in the ankle with the blood pressure in the arm.
- Ultrasound: Doppler ultrasound can help evaluate blood flow through the blood vessels.
- Angiography: Uses imaging techniques to view blood flow in the arteries.
- Blood Tests: To check for conditions related to PAD, such as diabetes and high cholesterol.
Treatment of Peripheral Artery Disease (PAD)
Treatment for Peripheral Artery Disease (PAD) aims to manage symptoms and prevent complications. It include:
- Lifestyle Changes: Quitting smoking, eating a healthy diet, and exercising regularly.
- Medications: To lower cholesterol, control blood pressure and blood sugar, prevent blood clots, and relieve symptoms.
- Angioplasty and Surgery: In severe cases, procedures to open blocked arteries or bypass them.
- Supervised Exercise Programs: Improve symptoms and increase walking distance.
Lifestyle Changes for Managing Peripheral Artery Disease (PAD)
Making healthy lifestyle changes is a critical component of managing Peripheral Artery Disease (PAD). Key changes include:
- Quit Smoking: Smoking cessation is the most important step to reduce the risk of PAD progression.
- Healthy Diet: Eating a diet rich in fruits, vegetables, whole grains, and lean proteins helps manage cholesterol and blood pressure.
- Regular Exercise: A supervised exercise program can improve symptoms and increase walking distance.
- Weight Management: Maintaining a healthy weight reduces the strain on your heart and blood vessels.
- Control Blood Sugar: For people with diabetes, controlling blood sugar is essential to prevent complications.
Medications for Peripheral Artery Disease (PAD)
Several medications can help manage Peripheral Artery Disease (PAD) and its risk factors. These include:
- Antiplatelet Agents: Such as aspirin to prevent blood clots.
- Cholesterol-Lowering Medications: Such as statins to manage cholesterol levels.
- Blood Pressure Medications: To control high blood pressure.
- Medications for Symptom Relief: Cilostazol or pentoxifylline to improve walking distance.
Surgical and Non-Surgical Procedures for PAD
In some cases, surgical or non-surgical procedures may be necessary to treat Peripheral Artery Disease (PAD). These include:
- Angioplasty: A minimally invasive procedure to open narrowed or blocked arteries.
- Stenting: Placement of a small wire mesh tube to keep the artery open.
- Bypass Surgery: Creating a detour around the blocked artery using a graft.
- Atherectomy: Removing plaque from the arteries.
Peripheral Artery Disease (PAD) and Exercise
Regular exercise is crucial for managing Peripheral Artery Disease (PAD). Exercise helps improve symptoms, increase walking distance, and enhance overall cardiovascular health. A supervised exercise program, often referred to as a structured walking program, is particularly effective. This involves walking until moderate pain is felt, resting until the pain subsides, and then repeating the process.
Peripheral Artery Disease (PAD) and Diet
Diet plays a significant role in managing Peripheral Artery Disease (PAD). A heart-healthy diet can help control risk factors such as high cholesterol, high blood pressure, and obesity. Key dietary recommendations include:
- Increase Fruits and Vegetables: These are rich in vitamins, minerals, and fiber.
- Choose Whole Grains: Whole grains are better for heart health than refined grains.
- Limit Saturated and Trans Fats: These fats can raise cholesterol levels.
- Reduce Sodium: Helps control blood pressure.
- Lean Proteins: Such as fish, poultry, beans, and legumes.

Preventing Peripheral Artery Disease (PAD)
Preventing Peripheral Artery Disease (PAD) involves managing risk factors and adopting a healthy lifestyle. Important preventive measures include:
- Don’t Smoke: Avoid smoking and seek help to quit if you do.
- Healthy Diet: Eat a balanced diet low in saturated fats, cholesterol, and sodium.
- Regular Physical Activity: Aim for at least 30 minutes of moderate exercise most days.
- Maintain a Healthy Weight: Reduce strain on your heart and blood vessels.
- Manage Chronic Conditions: Control conditions like diabetes, high blood pressure, and high cholesterol.
Complications of Peripheral Artery Disease
If left untreated, Peripheral Artery Disease can lead to serious complications, including:
- Critical Limb Ischemia (CLI): Severe blockage in the arteries that can lead to sores, infections, and tissue death.
- Heart Attack and Stroke: Increased risk due to systemic atherosclerosis.
- Amputation: Severe PAD can lead to tissue death and the need for amputation.
Peripheral Artery Disease in Special Populations
Certain populations are at higher risk of Peripheral Artery Disease, including:
- Diabetics: Diabetes significantly increases the risk of PAD and its complications.
- Elderly: The risk of PAD increases with age.
- Women: Women may experience different symptoms than men and are often underdiagnosed.
- Ethnic Minorities: Higher prevalence of PAD in certain ethnic groups, including African Americans.
Living with Peripheral Artery Disease
Living with Peripheral Artery Disease requires ongoing management and lifestyle adjustments. Key strategies include:
- Regular Medical Checkups: Monitor the progression of PAD and adjust treatment as needed.
- Medication Adherence: Take prescribed medications regularly.
- Healthy Lifestyle: Maintain a healthy diet, exercise regularly, and avoid smoking.
- Monitor Symptoms: Report any new or worsening symptoms to your healthcare provider promptly.
The Importance of Early Detection
Early detection of Peripheral Artery Disease is crucial for effective management and prevention of complications. Regular checkups, especially if you have risk factors for PAD, can help detect the condition early. Simple tests like the Ankle-Brachial Index (ABI) can be performed during routine visits to screen for PAD.
Future Directions in Peripheral Artery Disease Research
Research on Peripheral Artery Disease continues to advance, with ongoing studies aimed at improving diagnosis, treatment, and prevention. Areas of focus include:
- New Medications: Developing more effective drugs to manage symptoms and slow disease progression.
- Improved Diagnostic Tools: Enhancing non-invasive methods for early detection.
- Lifestyle Interventions: Studying the impact of diet and exercise programs on PAD outcomes.
- Genetic Research: Understanding the genetic factors that contribute to PAD.
Peripheral Artery Disease and Mental Health
Living with Peripheral Artery Disease can take a toll on mental health, leading to anxiety, depression, and reduced quality of life. It’s important to address these aspects as part of a comprehensive treatment plan. Support groups, counseling, and mental health professionals can provide valuable assistance.
Community and Support for Peripheral Artery Disease
Support from the community and healthcare professionals is essential for managing Peripheral Artery Disease. Joining support groups, both online and offline, can provide emotional support, practical advice, and encouragement. Healthcare providers can offer resources and referrals to support services.
Peripheral Artery Disease and Occupational Health
Peripheral Artery Disease can affect work life, especially for those with physically demanding jobs. It’s important to discuss your condition with your employer and make necessary adjustments to your work routine. Ergonomic interventions, flexible schedules, and appropriate job roles can help manage PAD symptoms while maintaining employment.
Peripheral Artery Disease and Travel
Traveling with Peripheral Artery Disease requires careful planning to manage symptoms and prevent complications. Tips for traveling include:
- Plan Ahead: Schedule breaks to walk and stretch during long journeys.
- Medication Management: Carry enough medication and keep it in your carry-on luggage.
- Stay Hydrated: Drink plenty of water to maintain circulation.
- Wear Compression Stockings: To prevent blood clots during long flights or car rides.
FAQs
What are the main symptoms of Peripheral Artery Disease ?
Common symptoms of Peripheral Artery Disease include leg pain while walking (claudication), numbness, coldness in the lower leg or foot, and sores that won’t heal.
How is Peripheral Artery Disease diagnosed?
Peripheral Artery Disease is diagnosed through medical history, physical exams, and tests such as the Ankle-Brachial Index (ABI), ultrasound, angiography, and blood tests.
Can Peripheral Artery Disease be cured?
While there is no cure for Peripheral Artery Disease , it can be managed effectively with lifestyle changes, medications, and sometimes surgical procedures to improve blood flow.
What lifestyle changes can help manage Peripheral Artery Disease ?
Key lifestyle changes for managing Peripheral Artery Disease include quitting smoking, eating a healthy diet, exercising regularly, maintaining a healthy weight, and controlling blood sugar levels.
Are there any specific medications for Peripheral Artery Disease ?
Yes, medications for Peripheral Artery Disease include antiplatelet agents, cholesterol-lowering drugs, blood pressure medications, and drugs to relieve symptoms like claudication.
How can Peripheral Artery Disease complications be prevented?
Preventing complications involves managing risk factors, following treatment plans, regular medical checkups, and making healthy lifestyle choices.
Conclusion
Peripheral Artery Disease is a serious condition that requires early detection, comprehensive management, and ongoing lifestyle changes to prevent complications. By understanding the causes, risk factors, symptoms, and treatment options, individuals can take proactive steps to manage PAD and improve their quality of life. Regular checkups, adherence to treatment plans, and a commitment to a healthy lifestyle are essential for living well with Peripheral Artery Disease.

Our Doctors
Dedicated IR Center for Vascular Problems in Madhya Pradesh
DR. SHAILESH GUPTA
MD, PDCC (INTERVENTIONAL RADIOLOGY) Consultant & Co-Director CVIC (Center Of Vascular & Interventional Care)
DR. ALOK KUMAR UDIYA
MD Radiology, PDCC (Neurointervention Radiology), PDCC ( HPB Intervention Radiology) FINR (Switzerland) & EBIR
Endovascular Surgeon & Consultant Interventional Neuroradiologist at Care CHL Hospital, Indore Co-director CVIC( center for vascular and interventional care)
DR. NISHANT BHARGAVA
Consultant Intervention Radiologist
MD Radiology, PDCC ( Neurointervention Radiology), FINR ( Fellowship in Neurointervention Radiology)
Co-director CVIC(Center for Vascular and Interventional Care)
Contact Details
Phone no.
0731 4675670
+91 9827760073
Facebook
https://www.facebook.com/profile.php?id=100092538633553&mibextid=ZbWKwL
Instagram
https://instagram.com/cvic_center?igshid=ZGUzMzM3NWJiOQ==
Google My business
https://g.co/kgs/DrdV3T
YouTube
https://www.youtube.com/channel/UCP5TH5e4iQZkpDUgnLsgZhw
Pinterest
https://pin.it/5DzpX5Z
Twitter
https://x.com/cviccenter?t=01TclSrLFdu0K2re0Gs96w&s=08
LINKEDIN
https://www.linkedin.com/company/center-of-vascular-interventional-care/
Location –
Read More –
What is Perma Cath used for? – https://cvicvascular.com/perma-cath-used-for/
Is inserting chemo port painful? – https://cvicvascular.com/is-inserting-chemo-port-painful/
What is the difference between a kyphoplasty and vertebroplasty? – https://cvicvascular.com/kyphoplasty-vs-vertebroplasty-difference/