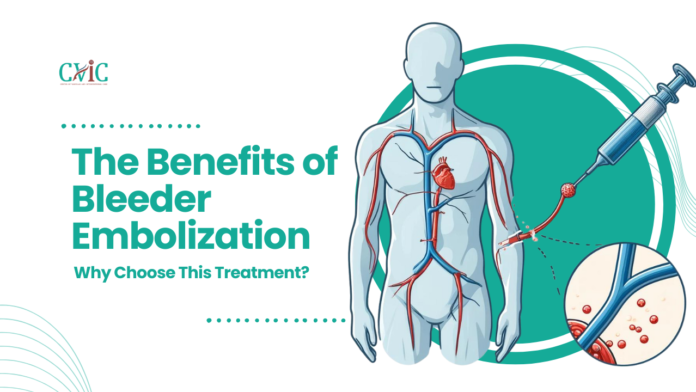
Bleeder embolization is a medical marvel that has transformed the treatment of internal bleeding. By strategically blocking the blood vessels responsible for bleeding, this minimally invasive procedure offers an effective and safe solution for various medical conditions. Understanding the benefits of bleeder embolization can help patients make informed decisions about their treatment options.
Introduction
In the world of modern medicine, innovative treatments have revolutionized patient care, offering less invasive and more effective solutions for complex health issues. One such innovation is bleeder embolization. This procedure has emerged as a game-changer in the management of internal bleeding, providing numerous benefits over traditional surgical methods. This article delves into the multifaceted advantages of bleeder embolization and why it stands out as a preferred treatment choice.
Understanding Bleeder Embolization
Bleeder embolization, also known as embolotherapy, is a procedure that involves the intentional blockage of blood vessels to control or prevent bleeding. It is performed using catheters and imaging techniques to guide the delivery of embolic agents to the target site. These agents can be coils, particles, or other materials designed to obstruct blood flow in the affected vessels.

Why Choose Bleeder Embolization?
Minimally Invasive Nature
One of the most significant advantages of bleeder embolization is its minimally invasive nature. Unlike traditional open surgery, embolization requires only small incisions, reducing the risk of complications, infection, and scarring. Patients experience less pain and a quicker recovery time, making it an attractive option for those looking to minimize downtime.
Effective Control of Bleeding
Bleeder embolization is highly effective in controlling bleeding, whether it is due to trauma, gastrointestinal issues, or other medical conditions. The precision with which the embolic agents are delivered ensures that the bleeding is stopped promptly, reducing the risk of severe blood loss and associated complications.
Targeted Treatment
The procedure allows for targeted treatment of the bleeding site. Using advanced imaging techniques, interventional radiologists can accurately locate the source of bleeding and deliver the embolic agents precisely where needed. This precision enhances the effectiveness of the treatment and minimizes damage to surrounding tissues.
Reduced Recovery Time
Patients undergoing bleeder embolization typically enjoy a much shorter recovery time compared to those undergoing traditional surgery. The minimally invasive approach means less physical trauma to the body, allowing patients to return to their normal activities sooner. This benefit is particularly important for individuals with busy lifestyles or those who cannot afford prolonged downtime.
Lower Risk of Complications
Traditional surgery carries inherent risks such as infection, blood clots, and complications from anesthesia. Bleeder embolization significantly reduces these risks due to its less invasive nature. The procedure is performed under local anesthesia, further minimizing the potential for adverse reactions and complications.
Versatility in Treating Various Conditions
Bleeder embolization is versatile and can be used to treat a wide range of conditions that cause internal bleeding. These include gastrointestinal bleeding, bleeding from tumors, trauma-induced bleeding, and vascular malformations. Its adaptability makes it a valuable tool in the medical field, providing solutions for conditions that might otherwise require more invasive treatments.
Improved Patient Outcomes
Studies have shown that patients who undergo bleeder embolization often experience better overall outcomes compared to those who receive traditional surgical treatments. The reduced risk of complications, shorter hospital stays, and faster recovery times contribute to improved patient satisfaction and quality of life.
Cost-Effectiveness
While the initial cost of bleeder embolization might be comparable to or slightly higher than traditional surgery, the overall cost-effectiveness is superior. The shorter hospital stay, reduced need for postoperative care, and quicker return to normal activities translate into lower healthcare costs in the long run. This economic advantage is beneficial for both patients and healthcare systems.
The Procedure: What to Expect
When considering bleeder embolization, it’s essential to understand the various steps involved in the procedure. Knowing what to expect can help alleviate anxiety and ensure a smoother experience. Here’s a detailed look at the stages of bleeder embolization from preparation to post-procedure care.
Pre-Procedure Preparation
Diagnostic Evaluation
Before undergoing bleeder embolization, a thorough diagnostic evaluation is conducted. This typically includes imaging studies such as:
- CT Scans: To get a detailed view of the internal structures and identify the source of bleeding.
- MRI: Provides a more comprehensive image of soft tissues and vascular structures.
- Angiography: An X-ray technique that uses a contrast dye to visualize blood vessels and pinpoint the bleeding site.
Medical History and Physical Examination
A comprehensive medical history and physical examination are necessary to ensure that the patient is a suitable candidate for the procedure. This includes:
- Reviewing Past Medical Conditions: Especially those related to bleeding disorders or previous surgeries.
- Medications: Discussing any current medications, as some may need to be adjusted or paused.
- Allergies: Noting any allergies, particularly to contrast dye or anesthesia.
Patient Instructions
Patients receive specific instructions to prepare for the procedure:
- Fasting: Usually, patients are required to fast for several hours before the procedure.
- Medication Adjustments: Some medications, particularly blood thinners, might need to be adjusted.
- Consent Form: Signing an informed consent form after discussing the procedure’s risks and benefits with the healthcare provider.

During the Procedure
Anesthesia and Sedation
The procedure is typically performed under local anesthesia with sedation. The patient remains awake but relaxed and pain-free.
Catheter Insertion
- Access Point: A small incision is made, usually in the groin area, to access the femoral artery. Alternatively, access can be gained through the radial artery in the wrist.
- Catheter Navigation: Using fluoroscopy (real-time X-ray imaging), the interventional radiologist threads a catheter through the vascular system to the site of bleeding.
Embolic Agent Delivery
Once the catheter is in place:
- Position Confirmation: The exact location of the bleeding vessel is confirmed using contrast dye.
- Embolic Agents: Embolic materials, such as coils, particles, or liquid agents, are carefully delivered through the catheter to block the blood vessel and stop the bleeding.
- Monitoring: The procedure is closely monitored to ensure the embolic agents are effectively placed and the bleeding is controlled.
Duration
The entire procedure typically takes about one to two hours, depending on the complexity and the location of the bleeding.
Post-Procedure Care
Recovery Monitoring
After the procedure, patients are moved to a recovery area where they are closely monitored for a few hours to ensure there are no immediate complications such as bleeding at the catheter insertion site or adverse reactions to the procedure.
Discharge Instructions
Most patients can go home the same day or after an overnight stay. Discharge instructions typically include:
- Activity Restrictions: Patients are advised to avoid strenuous activities and heavy lifting for a few days.
- Wound Care: Keeping the incision site clean and dry is crucial to prevent infection.
- Medication: Pain management and any other prescribed medications should be taken as directed.
Follow-Up Appointments
Patients will need follow-up visits with their healthcare provider to monitor the recovery process and assess the effectiveness of the embolization. Additional imaging studies may be performed to ensure the bleeding has been adequately controlled.
Potential Complications and How to Handle Them
While bleeder embolization is generally safe, patients should be aware of potential complications and know when to seek medical attention.
Possible Complications
- Bleeding or Hematoma: At the catheter insertion site.
- Infection: At the insertion site or internally.
- Allergic Reactions: To contrast dye or embolic materials.
- Non-Target Embolization: Unintentional blockage of non-target vessels, leading to tissue damage.
When to Seek Help
Patients should contact their healthcare provider if they experience:
- Severe Pain: Unmanageable with prescribed medications.
- Signs of Infection: Such as redness, swelling, or discharge at the incision site.
- Fever: Indicating a possible infection.
- Numbness or Weakness: In the limb where the catheter was inserted.
- Persistent Bleeding: At the catheter site.
Conclusion
Understanding what to expect during bleeder embolization—from preparation to recovery—can help patients feel more comfortable and confident about the procedure. This minimally invasive treatment offers significant benefits, including effective control of internal bleeding, reduced recovery times, and lower risk of complications. By following the pre- and post-procedure guidelines and maintaining open communication with healthcare providers, patients can achieve the best possible outcomes from bleeder embolization.
Bleeder Embolization: An Overview
Bleeder embolization, also known as embolotherapy, is a medical procedure used to treat internal bleeding by intentionally blocking the blood vessels responsible for the bleeding. This minimally invasive technique is performed by interventional radiologists and has become a cornerstone in the management of various types of internal hemorrhages.
Understanding the Procedure
The primary goal of bleeder embolization is to stop or reduce blood flow to a specific area, thereby controlling bleeding. This is achieved through the insertion of a catheter into the vascular system, typically via a small incision in the groin or arm. Using real-time imaging guidance, the catheter is navigated to the bleeding site. Once the target area is reached, embolic agents—such as coils, particles, or liquid embolic materials—are introduced to block the blood vessels.
Applications and Indications
Bleeder embolization is utilized in a wide range of clinical scenarios, including but not limited to:
- Trauma: In cases of severe trauma, such as liver or splenic injuries, embolization can control bleeding quickly, stabilizing the patient for further treatment or surgery if necessary.
- Vascular Malformations: Conditions like arteriovenous malformations (AVMs) and aneurysms can cause significant bleeding. Embolization is used to occlude the abnormal vessels and prevent hemorrhage.
- Tumor Bleeding: Tumors, especially those in the liver, kidney, or pelvis, may bleed due to their vascular nature.
Procedure Details
Preparation: Prior to the procedure, patients undergo various diagnostic tests, including blood work, imaging studies (CT, MRI, or angiography), and consultations to determine the suitability of embolization. Patients may need to fast and adjust medications as directed by their healthcare provider.
During the Procedure: The patient is usually awake but sedated. After the local anesthesia is administered, a small incision is made to access the blood vessel.
Post-Procedure Care: Following the embolization, patients are monitored for a few hours to ensure there are no immediate complications. Depending on the case, patients might be discharged the same day or may require a short hospital stay. Post-procedure instructions include activity restrictions and follow-up appointments to monitor recovery.
Benefits of Bleeder Embolization
Minimally Invasive: The procedure involves small incisions and less physical trauma compared to traditional surgery, leading to reduced pain, lower risk of infection, and minimal scarring.
Targeted Treatment: Embolization allows for precise targeting of the bleeding site, which enhances the effectiveness of the procedure and minimizes damage to surrounding tissues.
Reduced Recovery Time: Patients generally experience a quicker recovery period, allowing them to return to their daily activities sooner.
Lower Risk of Complications: Compared to open surgery, embolization carries fewer risks of complications such as infections, blood clots, and adverse reactions to anesthesia.
Effectiveness: Bleeder embolization has a high success rate in controlling bleeding, providing immediate and long-term relief for patients.
Conclusion
Bleeder embolization represents a significant advancement in the treatment of internal bleeding. Its minimally invasive nature, precision, and effectiveness make it a preferred option for many patients and healthcare providers. By understanding the procedure, its applications, and its benefits, patients can make informed decisions about their treatment options, ensuring better health outcomes and quality of life.
FAQs about Bleeder Embolization
How long does it take to recover from bleeder embolization?
Recovery time varies depending on the individual’s health and the complexity of the procedure. However, most patients can resume normal activities within a week.
Is bleeder embolization painful?
The procedure itself is not painful due to the use of local anesthesia. Some patients may experience mild discomfort at the catheter insertion site afterward, but this typically resolves within a few days.
How do I know if bleeder embolization is right for me?
A consultation with an interventional radiologist or a specialist in the relevant medical field is essential to determine if bleeder embolization is the best treatment option for your specific condition.
What are the alternatives to bleeder embolization?
Alternatives to bleeder embolization include traditional surgery, endoscopic treatments, and medication management. The choice of treatment depends on the cause and severity of the bleeding, as well as the patient’s overall health.

Conclusion
The benefits of bleeder embolization are numerous and significant, making it a highly effective and preferred treatment option for controlling internal bleeding. Its minimally invasive nature, effectiveness, targeted approach, and improved patient outcomes make it a standout choice in modern medicine. For those facing conditions that cause internal bleeding, bleeder embolization offers a promising solution with reduced risks and faster recovery times, enhancing both health and quality of life.
Our Doctors
Dedicated IR Center for Vascular Problems in Madhya Pradesh
DR. SHAILESH GUPTA
MD, PDCC (INTERVENTIONAL RADIOLOGY) Consultant & Co-Director CVIC (Center Of Vascular & Interventional Care)
DR. ALOK KUMAR UDIYA
MD Radiology, PDCC (Neurointervention Radiology), PDCC ( HPB Intervention Radiology) FINR (Switzerland) & EBIR
Endovascular Surgeon & Consultant Interventional Neuroradiologist at Care CHL Hospital, Indore Co-director CVIC( center for vascular and interventional care)
DR. NISHANT BHARGAVA
Consultant Intervention Radiologist
MD Radiology, PDCC ( Neurointervention Radiology), FINR ( Fellowship in Neurointervention Radiology)
Co-director CVIC(Center for Vascular and Interventional Care)
Contact Details
Phone no.
0731 4675670
+91 9827760073
Facebook
https://www.facebook.com/profile.php?id=100092538633553&mibextid=ZbWKwL
Instagram
https://instagram.com/cvic_center?igshid=ZGUzMzM3NWJiOQ==
Google My business
https://g.co/kgs/DrdV3T
YouTube
https://www.youtube.com/channel/UCP5TH5e4iQZkpDUgnLsgZhw
Pinterest
https://pin.it/5DzpX5Z
Twitter
https://x.com/cviccenter?t=01TclSrLFdu0K2re0Gs96w&s=08
LINKEDIN
https://www.linkedin.com/company/center-of-vascular-interventional-care/
Location –
Read More –
10 Essential Insights into the Indications and Problems of Intracranial Stenting – https://cvicvascular.com/indications-and-problems-of-intracranial-stenting/
Conquering Spinal AVMs: The Power of Embolization – https://cvicvascular.com/spinal-avm-embolization/
How much does AVM embolization cost? – https://cvicvascular.com/avm-embolization-cost/