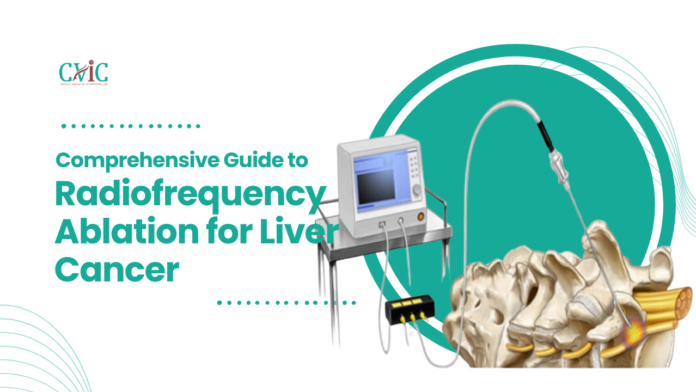
Radiofrequency Ablation (RFA) has emerged as a powerful tool in the arsenal against liver cancer, offering a minimally invasive alternative to traditional surgical procedures. This innovative treatment leverages the power of heat to destroy cancer cells, providing hope and improved outcomes for many patients. In this comprehensive guide, we will delve into the intricacies of RFA, exploring its benefits, procedure, effectiveness, and future directions.
Understanding Radiofrequency Ablation
Definition and Mechanism
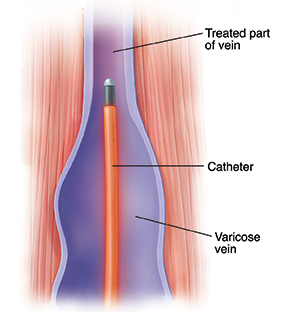
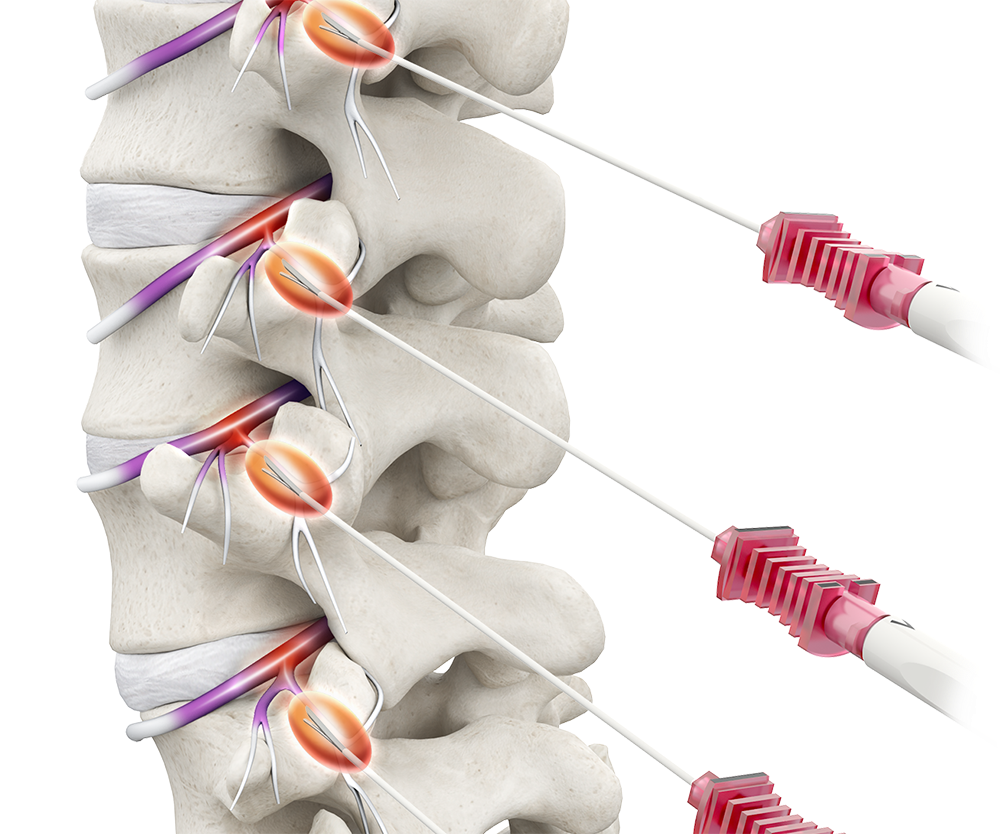
Radiofrequency Ablation is a minimally invasive procedure that uses high-frequency electrical currents to generate heat, which is then used to destroy cancer cells. This technique targets tumors in the liver by inserting a needle-like probe directly into the tumor. The probe emits radiofrequency energy, heating the surrounding tissue to temperatures high enough to cause cellular destruction.
Candidates for RFA
RFA is typically recommended for patients with early-stage liver cancer who are not suitable candidates for surgical resection or liver transplantation. This includes patients with small, localized tumors (generally less than 5 cm in diameter) and those with a limited number of tumors. RFA can also be used as a bridge therapy for patients awaiting liver transplantation, helping to control tumor growth and prevent disease progression.
The RFA Procedure: Step-by-Step
Pre-Procedure Preparation
Before undergoing RFA, patients undergo a thorough evaluation, including imaging studies such as CT scans or MRIs to precisely locate the tumor and assess its size and shape. Blood tests are also performed to evaluate liver function and overall health. On the day of the procedure, patients may be given a sedative and local anesthesia to ensure comfort and reduce pain during the treatment.
Insertion of the Probe
Once the patient is prepared, the interventional radiologist or oncologist uses imaging guidance to insert the RFA probe through the skin and into the liver tumor. The probe placement is critical, as it must be positioned accurately to ensure effective treatment while minimizing damage to surrounding healthy tissue.
Ablation Process
After the probe is correctly positioned, radiofrequency energy is delivered through the probe to the tumor. This energy generates heat, raising the temperature within the tumor to approximately 60 to 100 degrees Celsius. The heat causes coagulative necrosis, effectively killing the cancer cells and destroying the tumor. The duration of the ablation process can vary depending on the size and number of tumors being treated.
Post-Procedure Care
Following the ablation, the probe is removed, and the puncture site is covered with a sterile dressing. Patients are typically monitored for a few hours to ensure there are no immediate complications, such as bleeding or infection. Most patients can return home the same day, although they may need to rest and avoid strenuous activities for a few days.
Benefits of Radiofrequency Ablation
Radiofrequency Ablation (RFA) has revolutionized the treatment landscape for liver cancer, offering a minimally invasive, effective, and targeted option for patients. Here, we explore the numerous benefits of RFA, highlighting why it has become a preferred treatment modality for many.
Minimally Invasive Nature
Reduced Surgical Risk
RFA is performed through a small needle puncture rather than large surgical incisions. This minimally invasive approach significantly reduces the risk of complications associated with traditional surgery, such as infections, bleeding, and prolonged recovery times.
Shorter Hospital Stays
Patients undergoing RFA typically experience shorter hospital stays compared to those undergoing surgical resection. Many RFA procedures can be performed on an outpatient basis, allowing patients to return home the same day. This convenience is particularly beneficial for maintaining a normal lifestyle and reducing healthcare costs.
Quicker Recovery Time
The recovery time after RFA is much shorter than that following open surgery. Patients generally return to their normal activities within a few days to a week, compared to several weeks or months required for recovery from major surgery. This rapid recovery enhances the overall quality of life and reduces the emotional and physical stress associated with cancer treatment.
Targeted Treatment
Precision in Tumor Destruction
RFA allows for highly targeted treatment of liver tumors. The procedure involves inserting a probe directly into the tumor under imaging guidance, ensuring that the heat generated by radiofrequency energy is concentrated precisely on the cancer cells. This precision minimizes damage to surrounding healthy liver tissue, preserving liver function.
Effective for Small, Localized Tumors
For patients with small, localized liver tumors (generally less than 5 cm in diameter), RFA can achieve complete tumor destruction with high success rates. This makes RFA an excellent option for early-stage liver cancer patients who are not candidates for surgical resection or liver transplantation.
Effective Tumor Control
High Local Control Rates
Studies have demonstrated that RFA can achieve local control rates of up to 90% for tumors less than 3 cm in diameter. By effectively destroying the tumor cells, RFA can prevent local recurrence and manage disease progression, significantly enhancing patient outcomes.
Combination with Other Treatments
RFA can be combined with other treatments to improve its effectiveness. For instance, combining RFA with Transarterial Chemoembolization (TACE) can enhance tumor control in patients with larger or multiple tumors. Additionally, RFA can be part of a multimodal treatment approach that includes systemic therapies such as chemotherapy or targeted agents, further improving survival rates and quality of life.
Repeatable Procedure
Ongoing Cancer Management
One of the significant advantages of RFA is that it can be repeated multiple times if new tumors develop or if the initial treatment is not entirely successful. This repeatability allows for ongoing management of liver cancer, providing a flexible and adaptable treatment option that can be tailored to the patient’s evolving needs.
Adjunct to Other Therapies
RFA can serve as a bridge therapy for patients awaiting liver transplantation, helping to control tumor growth and prevent disease progression. It can also be used in conjunction with other ablative techniques such as microwave ablation or cryoablation, offering a comprehensive approach to liver cancer management.
Improved Quality of Life
Minimized Side Effects
Compared to systemic chemotherapy and other invasive treatments, RFA has a relatively low side effect profile. The localized nature of the treatment reduces systemic exposure to chemotherapy drugs, minimizing common side effects such as nausea, fatigue, and hair loss. This preservation of overall health is crucial for maintaining a high quality of life during cancer treatment.
Symptom Relief
For patients with symptomatic liver tumors, RFA can provide significant relief from symptoms such as pain, discomfort, and jaundice. By reducing the tumor burden, RFA can alleviate these symptoms, improving the patient’s overall well-being and daily functioning.
Advancements in Technology
Enhanced Imaging Techniques
Ongoing advancements in imaging technology, such as real-time ultrasound, CT, and MRI guidance, have significantly improved the precision and effectiveness of RFA. These imaging techniques allow for better visualization of the tumor and surrounding structures, ensuring accurate probe placement and optimal ablation outcomes.
Innovative Ablation Devices
The development of new ablation devices and probes has further enhanced the efficacy of RFA. For instance, multipolar and clustered electrodes can create larger ablation zones, making the treatment more effective for slightly larger tumors or tumors located in challenging areas. These technological innovations continue to expand the applicability and success rates of RFA.
Clinical Outcomes
Comparable to Surgical Resection
For selected patients with small, early-stage liver tumors, RFA has shown survival rates comparable to those achieved with surgical resection. This makes RFA a valuable alternative for patients who are not candidates for surgery due to comorbidities, advanced age, or other factors.
Long-Term Survival
Long-term survival rates for patients undergoing RFA are promising, particularly for those with early-stage disease. Five-year survival rates can range from 40% to 70%, depending on various factors such as tumor size, number, and patient health. These favorable outcomes highlight the potential of RFA as a life-extending treatment option.
Radiofrequency Ablation (RFA) offers numerous benefits for liver cancer patients, combining effectiveness with a minimally invasive approach. Its ability to provide targeted treatment, achieve high local control rates, and improve quality of life makes it an invaluable tool in the fight against liver cancer. As technology advances and new treatment combinations are explored, the role of RFA in liver cancer management will continue to grow, offering hope and better outcomes for patients worldwide.
Limitations and Challenges
Tumor Size and Location
RFA is most effective for small tumors (less than 5 cm) and may be less effective for larger tumors or those located near major blood vessels or other critical structures. The heat generated during the ablation can be dissipated by blood flow in larger vessels, reducing the effectiveness of the treatment.
Potential for Recurrence
While RFA is effective for localized tumor control, there is a potential for recurrence, particularly if microscopic cancer cells remain in the liver. Close monitoring and follow-up imaging are essential to detect and manage any recurrence promptly.
Not Suitable for All Patients
RFA is not suitable for all liver cancer patients. Those with advanced disease, multiple large tumors, or tumors located in challenging areas may not benefit from this treatment. Additionally, patients with severe liver dysfunction or other significant health issues may not be good candidates for RFA.
Side Effects and Complications
As with any medical procedure, RFA carries some risks and potential side effects. These can include pain at the insertion site, fever, infection, and damage to surrounding organs or structures. Serious complications are rare but can occur, underscoring the importance of having the procedure performed by experienced practitioners.
Effectiveness of Radiofrequency Ablation for Liver Cancer
Radiofrequency Ablation (RFA) has become an important tool in the treatment of liver cancer, particularly for patients who are not candidates for surgical resection or liver transplantation. This section delves into the effectiveness of RFA, examining survival rates, treatment outcomes, comparative effectiveness, and factors influencing the success of the procedure.
Survival Rates and Treatment Outcomes
High Local Control Rates
RFA is especially effective for small, localized tumors. Clinical studies have shown that RFA can achieve local control rates of up to 90% for tumors less than 3 cm in diameter. This high success rate in controlling the primary tumor significantly contributes to improved patient outcomes.
Survival Rates
For patients with early-stage liver cancer, RFA offers promising survival rates. Five-year survival rates for patients undergoing RFA can range from 40% to 70%, depending on factors such as tumor size, number, and the patient’s overall health. These survival rates are comparable to those achieved with surgical resection for small, solitary tumors, making RFA a viable alternative for many patients.
Disease-Free Survival
RFA also contributes to extended disease-free survival, which is the length of time after treatment that a patient remains free from cancer recurrence. Patients with smaller tumors and well-preserved liver function often experience longer disease-free intervals, enhancing their quality of life and reducing the need for additional treatments.
Factors Influencing Effectiveness
Tumor Size and Number
The size and number of tumors significantly impact the effectiveness of RFA. Smaller tumors (less than 5 cm) respond better to RFA, with higher rates of complete ablation and lower recurrence rates. Multiple or larger tumors present more challenges, and while RFA can still be effective, the outcomes are generally less favorable compared to single, small tumors.
Tumor Location
The location of the tumor within the liver is another critical factor. Tumors located near major blood vessels or bile ducts can be more difficult to treat effectively due to the risk of damaging these structures. Heat sink effect, where the blood flow in large vessels dissipates the heat generated by RFA, can reduce the effectiveness of the ablation.
Patient Health and Liver Function
Patients with good overall health and well-preserved liver function (Child-Pugh class A or B) have better outcomes with RFA. Those with decompensated liver disease (Child-Pugh class C) or severe comorbidities may not tolerate the procedure as well and may experience poorer outcomes.
Technical Expertise
The experience and skill of the practitioner performing RFA play a crucial role in the success of the procedure. Accurate probe placement and effective energy delivery are essential for achieving complete tumor ablation and minimizing complications. Institutions with experienced interventional radiologists or oncologists tend to report better outcomes.
Comparative Effectiveness
RFA vs. Surgical Resection
For patients with small, early-stage liver tumors, RFA has shown survival rates comparable to surgical resection. While surgical resection remains the gold standard for curative treatment, RFA provides a viable alternative for patients who are not suitable candidates for surgery due to comorbidities, advanced age, or other factors.
RFA vs. Other Ablation Techniques
Compared to other ablation techniques such as microwave ablation (MWA) and cryoablation, RFA has demonstrated similar effectiveness for small tumors. MWA, which uses microwave energy to generate heat, can create larger ablation zones and may be more effective for larger tumors. Cryoablation, which uses extreme cold to destroy cancer cells, is another alternative with comparable outcomes. The choice of technique often depends on tumor characteristics and the clinician’s expertise.
RFA Combined with Other Treatments
Combining RFA with other treatments, such as Transarterial Chemoembolization (TACE), systemic chemotherapy, or targeted therapies, can enhance its effectiveness. For instance, TACE can reduce tumor size and improve the efficacy of subsequent RFA by reducing the blood supply to the tumor. Combination therapies are particularly useful for patients with intermediate-stage liver cancer or those with tumors that are challenging to treat with RFA alone.
Long-Term Outcomes and Recurrence Rates
Recurrence Rates
While RFA is effective in achieving local control, there is a potential for recurrence, particularly in patients with larger tumors or those with multiple lesions. Recurrence can occur at the site of the original tumor or in other parts of the liver. Regular follow-up with imaging studies is essential to monitor for recurrence and manage it promptly if it occurs.
Long-Term Survival
Long-term survival for patients undergoing RFA is influenced by various factors, including tumor characteristics, liver function, and the presence of underlying liver disease such as cirrhosis. Patients with early-stage disease and good liver function can achieve long-term survival comparable to those undergoing surgical resection. Studies have shown that RFA can provide meaningful long-term survival benefits, particularly when used as part of a comprehensive treatment strategy.
Quality of Life
RFA is associated with improved quality of life for liver cancer patients. The minimally invasive nature of the procedure, coupled with its effectiveness in controlling tumors, allows patients to maintain their daily activities and reduces the physical and emotional burden of cancer treatment. Patients typically experience less pain and a quicker recovery compared to traditional surgery, enhancing their overall well-being.
Advancements and Future Directions
Technological Innovations
Advancements in imaging technology and ablation devices are continually improving the precision and effectiveness of RFA. Enhanced imaging modalities, such as real-time ultrasound, CT, and MRI, allow for better visualization of the tumor and surrounding structures, ensuring accurate probe placement and optimal ablation outcomes. Innovative ablation devices, such as multipolar and clustered electrodes, can create larger and more uniform ablation zones, expanding the applicability of RFA to larger and more complex tumors.
Personalized Medicine
The integration of genetic and molecular profiling into treatment planning is paving the way for personalized medicine in liver cancer treatment. By understanding the specific genetic and molecular characteristics of each patient’s tumor, clinicians can tailor RFA protocols and adjunctive treatments to enhance effectiveness and minimize side effects. Personalized treatment approaches are expected to improve outcomes and offer new hope for patients with liver cancer.
Combination Therapies
Research into combination therapies that integrate RFA with other treatments, such as immunotherapy and targeted agents, is ongoing. Immune checkpoint inhibitors, which have shown promise in various cancers, are being studied in combination with RFA to enhance the immune response against cancer cells. These combination strategies aim to provide more effective and durable tumor control, improving survival rates and quality of life for liver cancer patients.
Radiofrequency Ablation (RFA) is a highly effective treatment for liver cancer, offering a minimally invasive, targeted, and repeatable option for patients with small, localized tumors. The procedure’s effectiveness in achieving high local control rates, improving survival, and enhancing quality of life makes it an invaluable tool in the management of liver cancer. Ongoing advancements in technology and research into combination therapies and personalized treatment approaches promise to further enhance the effectiveness of RFA, providing better outcomes and new hope for patients worldwide.
Innovations and Future Directions of Radiofrequency Ablation for Liver Cancer
Advancements in Imaging and Technology
Ongoing advancements in imaging technology are improving the precision and effectiveness of RFA. Enhanced imaging modalities, such as fusion imaging that combines CT and ultrasound, allow for better visualization and targeting of tumors. Additionally, the development of real-time monitoring systems ensures that the ablation process is precisely controlled, optimizing treatment outcomes.
New Ablation Techniques
Researchers are exploring new ablation techniques and energy sources to improve the efficacy of RFA. Microwave ablation (MWA) and cryoablation are two such techniques that offer potential advantages over traditional RFA. MWA uses microwave energy to generate heat and destroy tumors, while cryoablation uses extreme cold to achieve the same effect. These alternative methods may provide more effective treatment for larger or difficult-to-reach tumors.
Personalized Treatment Approaches
The future of RFA and liver cancer treatment lies in personalized medicine. By integrating genetic and molecular profiling into treatment planning, clinicians can tailor RFA protocols to the individual characteristics of each patient’s cancer. This personalized approach aims to enhance the effectiveness of treatment, minimize side effects, and improve overall survival rates.
Combination with Immunotherapy
The combination of RFA with immunotherapy is an exciting area of research. Immunotherapy drugs, such as immune checkpoint inhibitors, can enhance the body’s immune response against cancer cells. When used in conjunction with RFA, which can release tumor antigens and stimulate an immune response, this combination could provide a powerful one-two punch against liver cancer.

FAQs
What is Radiofrequency Ablation?
Radiofrequency Ablation (RFA) is a minimally invasive procedure that uses high-frequency electrical currents to generate heat, which is then used to destroy cancer cells in the liver.
Who is a candidate for RFA?
RFA is typically recommended for patients with early-stage liver cancer who are not suitable candidates for surgical resection or liver transplantation, including those with small, localized tumors.
What are the benefits of RFA?
Benefits of RFA include its minimally invasive nature, targeted treatment, effective tumor control for small, localized tumors, and the ability to repeat the procedure if necessary.
What are the limitations of RFA?
Limitations include reduced effectiveness for larger tumors or those near major blood vessels, potential for recurrence, and unsuitability for patients with advanced disease or severe liver dysfunction.
How effective is RFA?
RFA can offer survival rates comparable to surgical resection for patients with small, localized tumors, with five-year survival rates ranging from 40% to 70%. It is also associated with improved quality of life.
What are the future directions for RFA?
Future directions include advancements in imaging and technology, new ablation techniques, personalized treatment approaches, and combination therapies with immunotherapy.
Conclusion
Radiofrequency Ablation (RFA) represents a significant advancement in the treatment of liver cancer, offering a minimally invasive, targeted, and effective option for many patients. While it has its limitations, ongoing innovations and research are continually enhancing its efficacy and expanding its applications. For patients with early-stage liver cancer, RFA provides hope for improved outcomes and a better quality of life, making it a vital component of modern oncology.
Our Doctors
Dedicated IR Center for Vascular Problems in Madhya Pradesh
DR. SHAILESH GUPTA
MD, PDCC (INTERVENTIONAL RADIOLOGY) Consultant & Co-Director CVIC (Center Of Vascular & Interventional Care)
DR. ALOK KUMAR UDIYA
MD Radiology, PDCC (Neurointervention Radiology), PDCC ( HPB Intervention Radiology) FINR (Switzerland) & EBIR
Endovascular Surgeon & Consultant Interventional Neuroradiologist at Care CHL Hospital, Indore Co-director CVIC( center for vascular and interventional care)
DR. NISHANT BHARGAVA
Consultant Intervention Radiologist
MD Radiology, PDCC ( Neurointervention Radiology), FINR ( Fellowship in Neurointervention Radiology)
Co-director CVIC(Center for Vascular and Interventional Care)
Contact Details
Phone no.
0731 4675670
+91 9827760073
Facebook
https://www.facebook.com/profile.php?id=100092538633553&mibextid=ZbWKwL
Instagram
https://instagram.com/cvic_center?igshid=ZGUzMzM3NWJiOQ==
Google My business
https://g.co/kgs/DrdV3T
YouTube
https://www.youtube.com/channel/UCP5TH5e4iQZkpDUgnLsgZhw
Pinterest
https://pin.it/5DzpX5Z
Twitter
https://x.com/cviccenter?t=01TclSrLFdu0K2re0Gs96w&s=08
LINKEDIN
https://www.linkedin.com/company/center-of-vascular-interventional-care/
Location –
Read More –
10 Essential Insights into the Indications and Problems of Intracranial Stenting – https://cvicvascular.com/indications-and-problems-of-intracranial-stenting/
Conquering Spinal AVMs: The Power of Embolization – https://cvicvascular.com/spinal-avm-embolization/
What is Perma Cath used for? – https://cvicvascular.com/perma-cath-used-for/