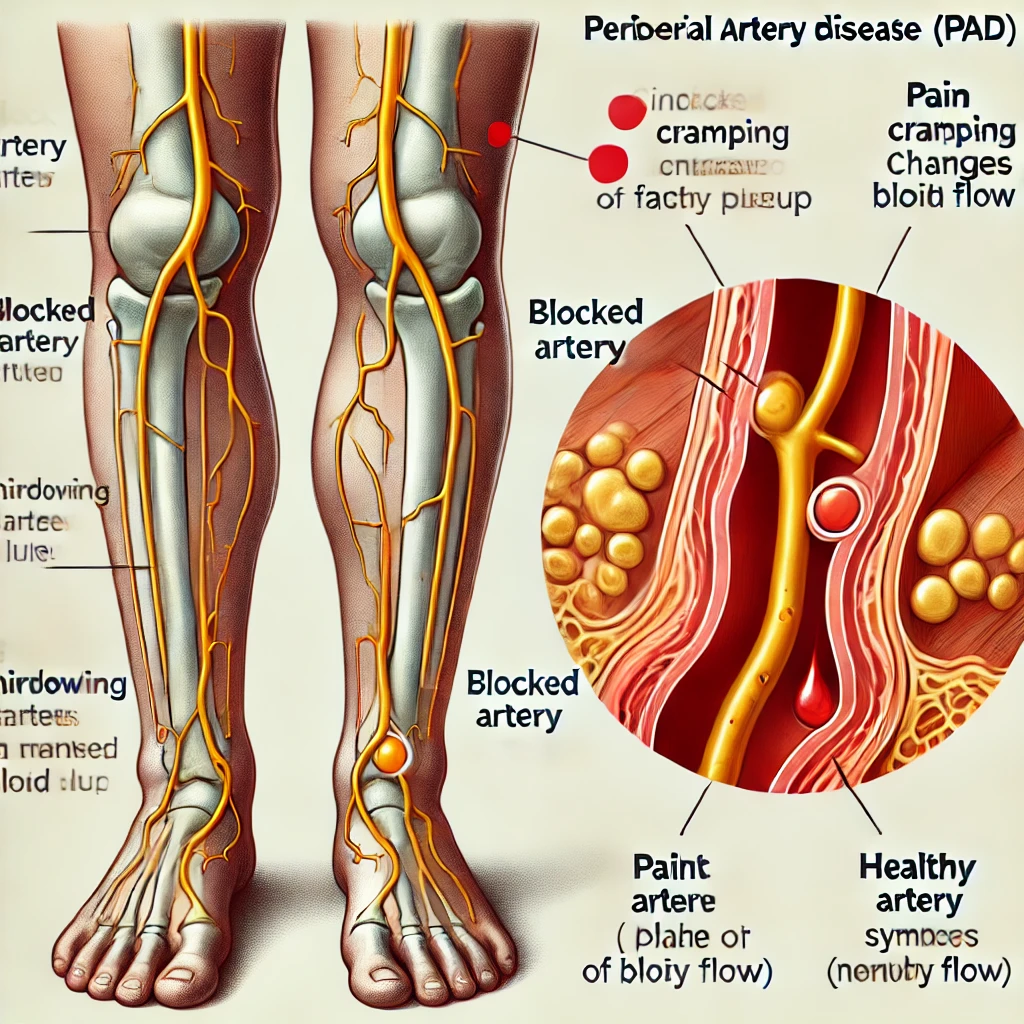
Peripheral Artery Disease (PAD) is a serious condition affecting the blood vessels outside the heart, particularly the arteries that supply blood to the limbs. As a common circulatory issue, PAD often leads to narrowed arteries, reducing blood flow to the extremities. This can result in leg pain while walking, known as claudication, and other serious complications if left untreated. But who is at risk for developing Peripheral Artery Disease (PAD)? Understanding the risk factors is crucial in preventing and managing this condition effectively.
What is Peripheral Artery Disease (PAD)?
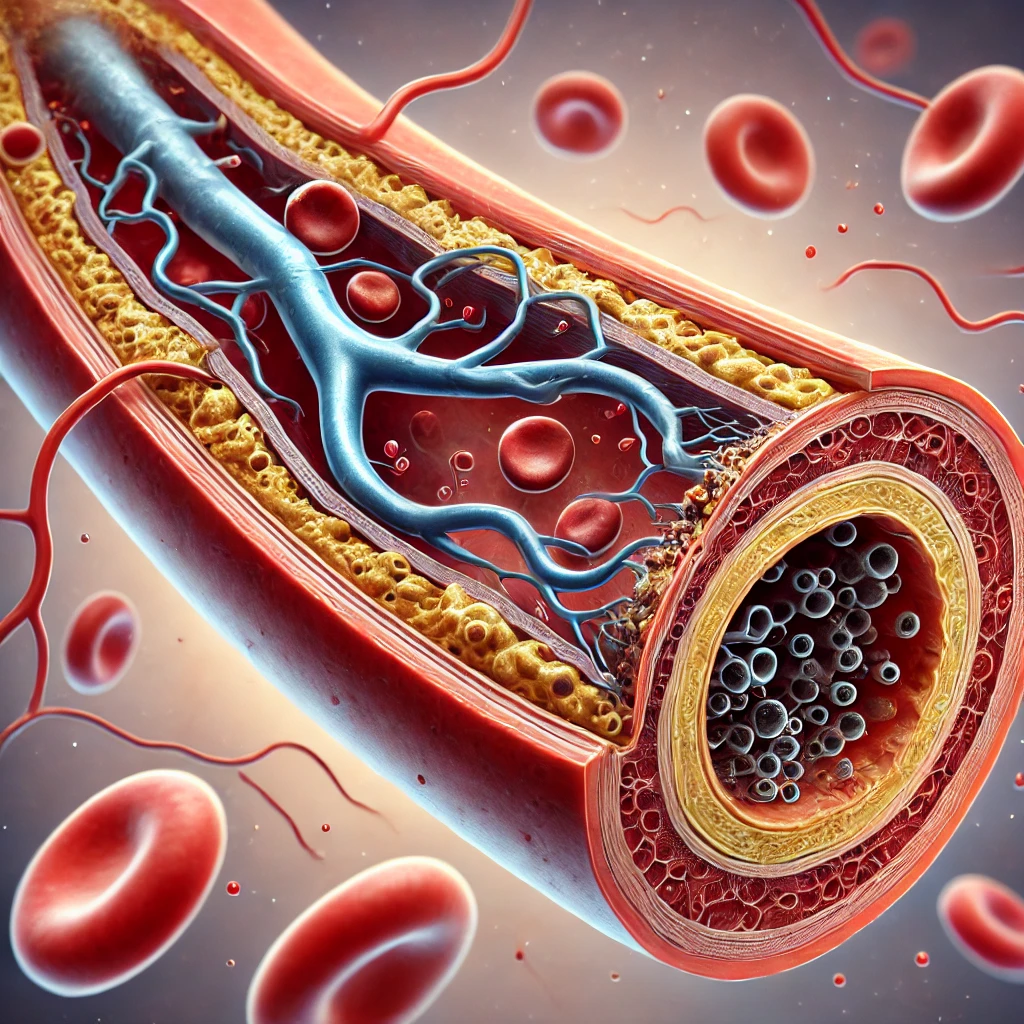
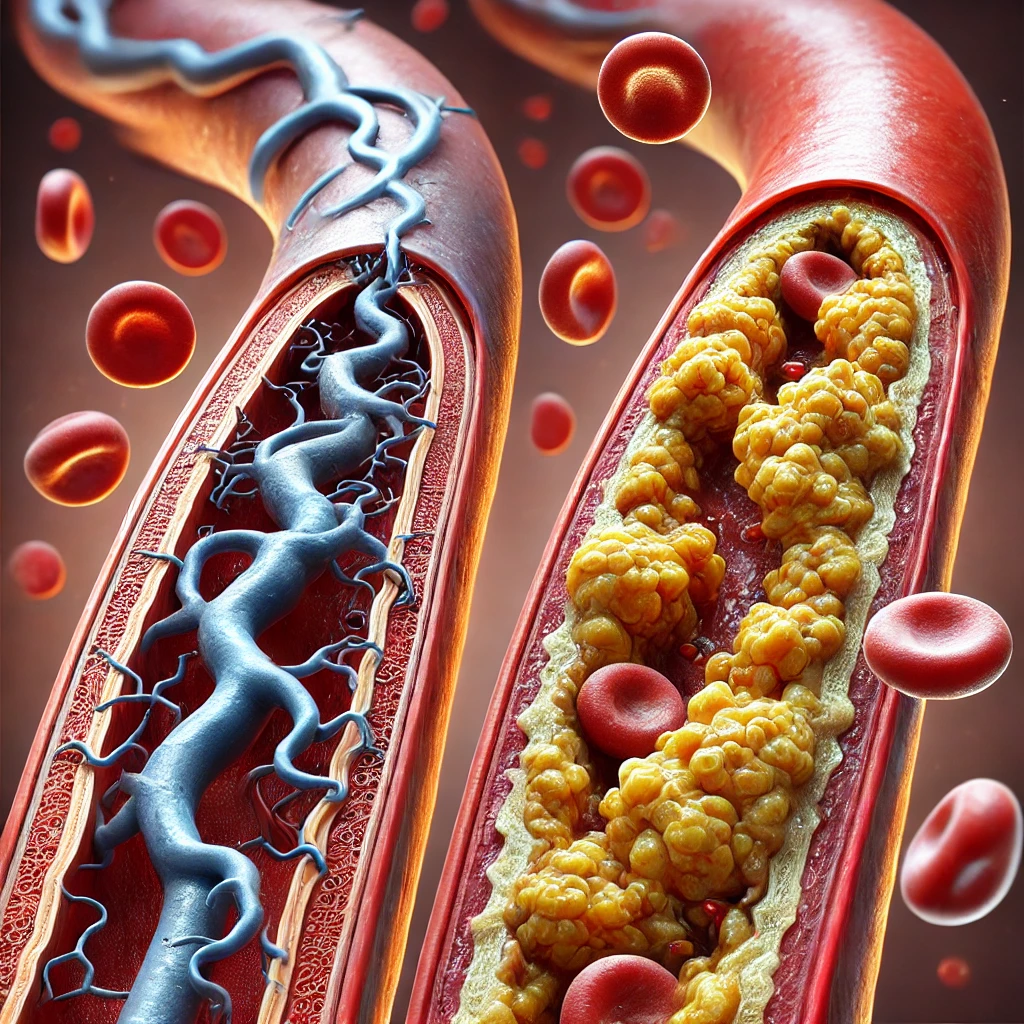
Peripheral Artery Disease (PAD) is a type of atherosclerosis, where plaque builds up in the arterial walls, narrowing the arteries and restricting blood flow. This condition primarily affects the arteries in the legs, but it can also impact other parts of the body. PAD is a progressive disease, meaning it can worsen over time if not addressed. Early diagnosis and treatment are key to improving outcomes and reducing the risk of severe complications such as heart attacks, strokes, or even limb amputation.
Why Understanding the Risk Factors for PAD is Important
Identifying who is most at risk for developing Peripheral Artery Disease (PAD) is essential for early detection and prevention. Knowing the risk factors can help individuals take proactive steps towards lifestyle changes, screenings, and medical interventions to manage their health. Let’s explore the primary risk factors associated with PAD.
Also Read: What Are the Benefits of Interventional Radiology?
Age and Peripheral Artery Disease (PAD)
As people age, the risk of developing Peripheral Artery Disease (PAD) increases significantly. The likelihood of PAD is higher in individuals over the age of 50, and the risk continues to rise with age. This is due to the natural aging process, which often leads to changes in the arteries, such as stiffening and plaque buildup.
Why Does Age Increase PAD Risk?
- Arterial Stiffness: With age, arteries naturally become less elastic, making it easier for plaque to accumulate and restrict blood flow.
- Prolonged Exposure to Risk Factors: The cumulative effect of other risk factors, such as high cholesterol and hypertension, over a lifetime contributes to the development of PAD.
Smoking: The Leading Modifiable Risk Factor for PAD
Smoking is one of the most significant risk factors for Peripheral Artery Disease (PAD). The chemicals in cigarettes damage the blood vessels, accelerate the buildup of plaque, and reduce the amount of oxygen in the blood, all of which increase the risk of PAD.
How Does Smoking Contribute to PAD?
- Increased Plaque Buildup: Smoking damages the inner lining of the arteries, making it easier for cholesterol and other substances to stick and form plaque.
- Reduced Oxygen Supply: Nicotine and carbon monoxide decrease the oxygen content in the blood, putting additional strain on the arteries.
- Inflammatory Response: Smoking triggers inflammation in the arteries, exacerbating the development of PAD.
Diabetes and Peripheral Artery Disease (PAD)
Diabetes is another major risk factor for developing Peripheral Artery Disease (PAD). High blood sugar levels damage the blood vessels and nerves over time, which can lead to atherosclerosis.
Also Read: What Treatment Options Are Available for Neurological Disorders?
Why Diabetics are at Higher Risk
- Elevated Blood Glucose Levels: High glucose levels can damage the arterial walls, promoting plaque formation.
- Nerve Damage: Diabetes often causes nerve damage (neuropathy), reducing the sensation in the feet and legs, making it harder for patients to notice PAD symptoms early.
- Increased Inflammation: Chronic inflammation from diabetes can accelerate the narrowing of the arteries.
High Blood Pressure and Peripheral Artery Disease (PAD)
Hypertension, or high blood pressure, is a critical risk factor for PAD. When blood pressure is consistently high, it exerts excessive force against the arterial walls, which can damage the arteries and lead to plaque buildup.
How Does Hypertension Contribute to PAD?
- Arterial Damage: High blood pressure can weaken the artery walls, making them more susceptible to atherosclerosis.
- Plaque Development: The damage caused by hypertension accelerates the buildup of fatty deposits, restricting blood flow.
- Increased Heart Workload: The heart has to work harder to pump blood through narrowed arteries, worsening the effects of PAD.
Obesity and Peripheral Artery Disease (PAD)
Obesity significantly raises the risk of developing Peripheral Artery Disease (PAD) due to the associated increase in cholesterol levels, blood pressure, and inflammation.
The Role of Obesity in PAD
- Higher Cholesterol Levels: Excess body fat contributes to higher cholesterol, increasing plaque buildup in the arteries.
- Elevated Inflammatory Markers: Obesity is linked with chronic inflammation, which can accelerate the development of atherosclerosis.
- Reduced Physical Activity: Obesity often leads to a sedentary lifestyle, which is another risk factor for PAD.
High Cholesterol: A Silent Risk Factor for PAD
High levels of cholesterol in the blood can lead to the buildup of plaque in the arteries, increasing the risk of Peripheral Artery Disease (PAD). This is often asymptomatic until significant narrowing occurs, making regular screening important.
How Cholesterol Affects the Arteries
- Plaque Formation: Excess LDL cholesterol deposits in the arterial walls, contributing to atherosclerosis.
- Reduced Arterial Elasticity: The buildup of plaque makes the arteries less flexible, increasing the risk of blockages.
- Inflammation: High cholesterol levels can trigger inflammation, further damaging the arteries.
Family History and Genetic Factors
If you have a family history of atherosclerosis or cardiovascular diseases, your risk of developing Peripheral Artery Disease (PAD) is higher. Genetics can play a significant role in how your body processes cholesterol and handles arterial health.
Lifestyle Choices and Peripheral Artery Disease (PAD)
Unhealthy lifestyle choices, such as poor diet, lack of exercise, and excessive alcohol consumption, can significantly increase the risk of PAD. A diet high in saturated fats and sugars contributes to obesity and high cholesterol, while a sedentary lifestyle reduces blood circulation.
Also Read: Best Treatment for an Aneurysm: Key Options to Consider for Optimal Recovery
Ethnic and Racial Factors
Certain racial and ethnic groups are more prone to developing Peripheral Artery Disease (PAD). African Americans, in particular, have a higher prevalence of PAD compared to other groups, partly due to higher rates of diabetes and hypertension.
Conclusion
Peripheral Artery Disease is a serious condition influenced by a range of factors, including age, smoking, diabetes, high blood pressure, obesity, high cholesterol, and family history. Understanding these risk factors is the first step in prevention and early intervention. Regular screenings, lifestyle changes, and medical management can help reduce the risk and manage the symptoms of PAD effectively.
FAQs
Who is most likely to develop Peripheral Artery Disease?
Individuals over the age of 50, smokers, diabetics, and those with a family history of cardiovascular diseases are at higher risk.
Can lifestyle changes reduce the risk of PAD?
Yes, quitting smoking, maintaining a healthy weight, and exercising regularly can significantly lower the risk of PAD.
Is Peripheral Artery Disease reversible?
While PAD is not fully reversible, lifestyle changes and medications can help manage symptoms and slow its progression.
How is Peripheral Artery Disease diagnosed?
PAD is typically diagnosed through a physical examination, ankle-brachial index (ABI) test, and imaging studies like ultrasound.
What are common symptoms of PAD?
Common symptoms include leg pain, cramping, numbness, and sores that heal slowly on the legs and feet.
Can high blood pressure alone cause Peripheral Artery Disease?
High blood pressure increases the risk of PAD but usually works in combination with other factors like smoking and high cholesterol.