Thrombolysis is a medical treatment designed to dissolve dangerous clots in blood vessels, improve blood flow, and prevent damage to tissues and organs. This procedure is especially critical in emergency situations, such as during a heart attack or stroke, where rapid restoration of blood flow can save lives and minimize long-term damage. In this detailed guide, we will explore the thrombolysis procedure, its benefits, potential risks, and its effectiveness in various clinical scenarios.
What is Thrombolysis?
Definition and Purpose
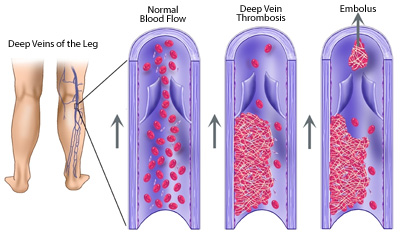
Thrombolysis, also known as fibrinolytic therapy, involves the administration of medication to dissolve blood clots that obstruct blood vessels. These clots can lead to severe conditions such as myocardial infarction (heart attack), ischemic stroke, deep vein thrombosis (DVT), and pulmonary embolism.
Types of Thrombolytic Agents
- Tissue Plasminogen Activator (tPA): The most commonly used thrombolytic agent, tPA, is a protein involved in the breakdown of blood clots.
- Streptokinase: An enzyme that helps dissolve clots but is less commonly used due to potential allergic reactions.
- Urokinase: Another enzyme used to break down clots, often utilized in catheter-directed thrombolysis.

Thrombolysis Procedure
Intravenous Thrombolysis
Administration: In intravenous thrombolysis, the thrombolytic agent is administered through an IV line directly into the bloodstream. This method is often used in emergency settings, such as treating a heart attack or ischemic stroke, where rapid clot dissolution is crucial.
Procedure Overview
- Diagnosis: Quick imaging tests, such as CT or MRI scans, confirm the presence of a clot.
- Medication Delivery: The thrombolytic agent is infused through an IV line over a set period, typically an hour.
- Monitoring: Patients are closely monitored for signs of improved blood flow and potential complications.
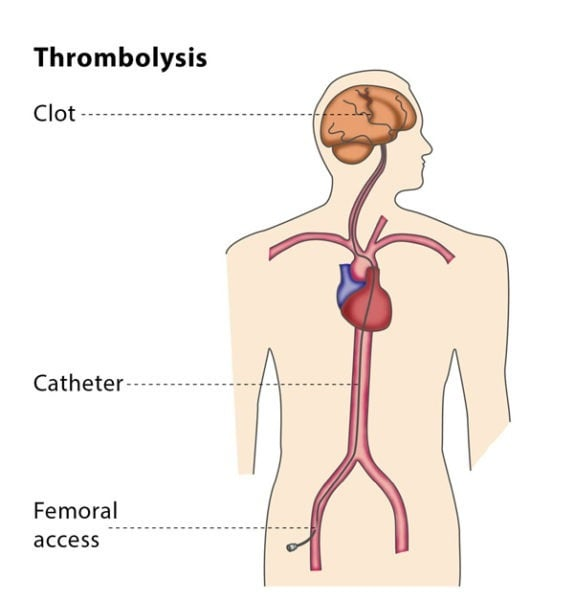
Catheter-Directed Thrombolysis
Targeted Treatment: Catheter-directed thrombolysis involves threading a catheter through the blood vessels to the site of the clot. The thrombolytic agent is then delivered directly to the clot, allowing for targeted treatment and potentially lower doses of medication.
Procedure Overview
- Imaging Guidance: Ultrasound or fluoroscopy is used to guide the catheter to the clot.
- Catheter Insertion: A small incision is made, and the catheter is inserted into a blood vessel, usually in the groin or arm.
- Medication Delivery: The thrombolytic agent is delivered directly to the clot through the catheter.
- Clot Dissolution: The clot dissolves over several hours to days, depending on the size and location of the clot.
- Follow-Up Imaging: Additional imaging tests ensure the clot has dissolved and blood flow is restored.
Benefits of Thrombolysis
Thrombolysis, also known as fibrinolytic therapy, is a critical medical treatment that offers significant benefits in managing and resolving blood clots. This treatment is particularly valuable in emergencies such as heart attacks and ischemic strokes, where rapid intervention can save lives and reduce long-term damage. Below, we explore the numerous benefits of thrombolysis in detail, highlighting its importance in modern medical practice.
Rapid Restoration of Blood Flow
Immediate Effectiveness: One of the most significant benefits of thrombolysis is its ability to quickly dissolve blood clots and restore blood flow. In cases of myocardial infarction (heart attack) or ischemic stroke, time is of the essence. Thrombolytic agents such as tissue plasminogen activator (tPA) can begin to dissolve clots within minutes of administration, significantly improving the chances of survival and recovery.
Life-Saving Intervention: In the context of a heart attack, restoring blood flow to the heart muscle can prevent extensive damage and preserve heart function. Similarly, in an ischemic stroke, re-establishing blood flow to the brain can prevent widespread brain damage and improve neurological outcomes.
Reduced Tissue Damage
Minimizing Ischemic Injury: Blood clots can block blood flow to vital organs and tissues, leading to ischemia and subsequent tissue damage. By dissolving these clots promptly, thrombolysis helps minimize ischemic injury, thereby preserving the function of affected organs. For instance, during a heart attack, thrombolysis can limit the extent of heart muscle damage, reducing the risk of heart failure and other complications.
Improved Organ Function: Preserving organ function is crucial for overall health and quality of life. Thrombolysis can help maintain the functionality of the heart, brain, and other organs by preventing prolonged periods of oxygen deprivation and nutrient deficiency caused by blood clots.
Enhanced Survival Rates
Higher Survival in Emergencies: Thrombolysis has been shown to significantly improve survival rates in patients experiencing acute medical emergencies such as heart attacks and strokes. Studies have demonstrated that early administration of thrombolytic therapy can reduce mortality rates and improve long-term outcomes for these patients.
Preventing Long-Term Disabilities: In the case of ischemic stroke, thrombolysis can prevent the severe neurological deficits that often result from prolonged brain ischemia. Patients who receive timely thrombolytic therapy are more likely to regain independence and experience fewer long-term disabilities compared to those who do not receive such treatment.
Non-Surgical Treatment Option
Minimally Invasive Approach: Thrombolysis offers a non-surgical alternative to traditional surgical interventions for blood clots, such as thrombectomy. This minimally invasive approach reduces the risks associated with surgery, such as infection, anesthesia complications, and prolonged recovery times.
Outpatient Possibilities: In some cases, thrombolysis can be administered in an outpatient setting, reducing the need for hospital stays and allowing patients to return to their daily activities more quickly. This is particularly beneficial for patients with less severe thromboembolic events or those at high risk for surgical complications.
Versatility in Application
Wide Range of Conditions: Thrombolysis is effective in treating a variety of thromboembolic conditions, including myocardial infarction, ischemic stroke, deep vein thrombosis (DVT), and pulmonary embolism. Its versatility makes it a valuable tool in the management of multiple types of blood clots.
Customizable Treatment: Different thrombolytic agents and delivery methods (such as intravenous infusion or catheter-directed administration) allow healthcare providers to tailor treatment to the specific needs and conditions of each patient. This customization enhances the effectiveness and safety of the therapy.
Improved Quality of Life
Symptom Relief: By resolving blood clots and restoring normal blood flow, thrombolysis can alleviate the painful and debilitating symptoms associated with thromboembolic conditions. For example, patients with DVT may experience relief from swelling and pain, while those with pulmonary embolism may find it easier to breathe.
Enhanced Daily Functioning: Reducing the physical and emotional burden of thromboembolic conditions can significantly improve patients’ quality of life. By preventing long-term complications and promoting recovery, thrombolysis helps patients maintain their independence and enjoy a better quality of life.
Prevention of Complications
Avoiding Severe Outcomes: By rapidly addressing blood clots, thrombolysis can prevent severe complications such as stroke, heart failure, pulmonary hypertension, and post-thrombotic syndrome. These complications can lead to chronic health issues and diminished quality of life if not promptly treated.
Supporting Long-Term Health: Effective thrombolysis supports long-term health by reducing the risk of recurrent thromboembolic events. Patients who undergo successful thrombolysis are less likely to experience future clots, thanks to improved blood flow and continued medical management.
Risks and Complications
Bleeding
The most significant risk associated with thrombolysis is bleeding, as the medication used to dissolve clots can also interfere with normal blood clotting processes. This can lead to internal bleeding, including gastrointestinal bleeding or intracranial hemorrhage.
Allergic Reactions
Although rare, some patients may experience allergic reactions to thrombolytic agents, particularly streptokinase. Symptoms can include rash, itching, swelling, or difficulty breathing.
Recurrent Clot Formation
There is a risk that new clots may form after the initial clot is dissolved. This necessitates ongoing monitoring and potentially additional treatments to prevent recurrence.
Effectiveness of Thrombolysis
Thrombolysis is a critical medical intervention for the dissolution of blood clots, which can obstruct blood flow and lead to severe health conditions such as heart attacks, strokes, and pulmonary embolisms. Evaluating the effectiveness of thrombolysis involves considering its success in different clinical scenarios, the speed and completeness of clot resolution, the improvement in patient outcomes, and its role in both emergency and elective settings. This detailed analysis highlights the factors contributing to the effectiveness of thrombolysis and its impact on patient care.
Clinical Scenarios for Thrombolysis
Myocardial Infarction (Heart Attack)
Rapid Clot Dissolution: In cases of myocardial infarction, thrombolysis is particularly effective when administered promptly. The primary goal is to dissolve the clot obstructing the coronary artery, thereby restoring blood flow to the heart muscle. This rapid clot dissolution helps to minimize myocardial damage and preserve heart function.
Timing is Crucial: The effectiveness of thrombolysis in heart attacks is highly dependent on the timing of administration. Studies show that thrombolytic therapy administered within the first 30 minutes to an hour of symptom onset significantly reduces mortality rates and improves long-term outcomes.
Improvement in Heart Function: Patients receiving timely thrombolysis often experience better preservation of heart function, reduced incidence of heart failure, and lower rates of recurrent heart attacks.
Ischemic Stroke
Neurological Outcomes: For ischemic strokes, thrombolysis using tissue plasminogen activator (tPA) is a standard treatment. The primary aim is to dissolve the clot blocking blood flow to the brain, thereby preventing extensive brain damage. The effectiveness of thrombolysis in this context is measured by improvements in neurological function and reduction in stroke-related disabilities.
Critical Time Window: The effectiveness of thrombolysis in stroke patients is highly time-sensitive. The best outcomes are observed when thrombolysis is initiated within 3 to 4.5 hours of symptom onset. Delayed treatment can significantly reduce the therapy’s effectiveness and increase the risk of hemorrhagic complications.
Functional Recovery: Patients treated with thrombolysis within the optimal time window often show substantial recovery in motor and cognitive functions, leading to a higher likelihood of returning to independent living and reducing the need for long-term rehabilitation.
Effectiveness in Deep Vein Thrombosis and Pulmonary Embolism
Deep Vein Thrombosis (DVT)
Preventing Post-Thrombotic Syndrome: Thrombolysis is effective in treating severe cases of DVT, particularly when there is significant risk of post-thrombotic syndrome, which can cause chronic pain, swelling, and ulcers. By dissolving the clot, thrombolysis can restore normal blood flow and prevent these long-term complications.
Improving Vein Function: Successful thrombolysis in DVT can help preserve the function of affected veins, reducing the risk of chronic venous insufficiency and enhancing overall leg health.
Pulmonary Embolism (PE)
Reducing Mortality: In life-threatening cases of pulmonary embolism, thrombolysis is a critical intervention. By dissolving the clot in the pulmonary arteries, thrombolysis reduces the strain on the heart and improves oxygenation, thereby lowering the risk of death.
Enhancing Respiratory Function: Patients who undergo thrombolysis for pulmonary embolism often experience significant improvement in respiratory function, which can alleviate symptoms such as shortness of breath and chest pain.
Factors Influencing Thrombolysis Effectiveness
Patient Selection
Eligibility Criteria: The effectiveness of thrombolysis largely depends on selecting the right patients for treatment. Ideal candidates are those with confirmed thromboembolic events who meet specific criteria, such as the timing of symptom onset, overall health, and absence of contraindications like recent surgery or severe bleeding disorders.
Contraindications: Understanding contraindications is crucial. Patients with high risk of bleeding, recent surgeries, or certain medical conditions may not be suitable for thrombolysis, as the risks could outweigh the benefits.
Dosage and Administration
Optimal Dosage: Administering the correct dosage of thrombolytic agents is vital for maximizing effectiveness and minimizing adverse effects. Overdosage can lead to serious bleeding complications, while underdosage may result in incomplete clot dissolution.
Delivery Method: The method of delivery—whether intravenous or catheter-directed—can also influence the effectiveness of thrombolysis. Catheter-directed thrombolysis, for example, allows for targeted treatment of clots, potentially requiring lower doses and reducing systemic exposure to the thrombolytic agent.
Monitoring and Post-Treatment Care
Close Monitoring: Effective thrombolysis requires close monitoring during and after the procedure. Monitoring for signs of bleeding, allergic reactions, and ensuring that the clot is dissolving as expected is critical for patient safety and treatment success.
Follow-Up Care: Post-thrombolysis care involves ongoing evaluation to prevent recurrence of thromboembolic events. This may include anticoagulant therapy, lifestyle modifications, and regular medical check-ups to manage underlying risk factors.
Patient Selection and Contraindications
Criteria for Thrombolysis
Not all patients are suitable candidates for thrombolysis. Ideal candidates are those with a confirmed clot who meet specific criteria regarding the timing of symptom onset, overall health, and risk factors for bleeding.
Contraindications
- Recent Surgery: Patients who have recently undergone major surgery are at higher risk of bleeding complications.
- Bleeding Disorders: Individuals with known bleeding disorders or those on anticoagulant therapy may not be suitable for thrombolysis.
- Severe Hypertension: Uncontrolled high blood pressure increases the risk of intracranial hemorrhage.
Post-Thrombolysis Care
Monitoring and Follow-Up
After thrombolysis, patients require close monitoring to detect any signs of bleeding or recurrent clot formation. Follow-up imaging tests ensure the clot has dissolved, and blood flow is restored.
Additional Treatments
In some cases, additional treatments such as anticoagulant therapy or placement of a vena cava filter may be necessary to prevent new clots from forming.
Lifestyle Modifications
Patients are often advised to make lifestyle changes to reduce the risk of future clots. This includes maintaining a healthy diet, regular exercise, smoking cessation, and managing underlying conditions such as diabetes and hypertension.
Conclusion
Thrombolysis is a powerful and life-saving treatment for dissolving dangerous blood clots and restoring normal blood flow. While it carries certain risks, its benefits in emergency situations such as heart attacks, strokes, and severe thromboembolic events are significant. Understanding the procedure, its benefits, and potential complications can help patients and healthcare providers make informed decisions and optimize treatment outcomes. Through careful patient selection and diligent post-procedure care, thrombolysis can significantly improve survival rates and quality of life for those affected by severe blood clots.
Our Doctors
Dedicated IR Center for Vascular Problems in Madhya Pradesh
DR. SHAILESH GUPTA
MD, PDCC (INTERVENTIONAL RADIOLOGY) Consultant & Co-Director CVIC (Center Of Vascular & Interventional Care)
DR. ALOK KUMAR UDIYA
MD Radiology, PDCC (Neurointervention Radiology), PDCC ( HPB Intervention Radiology) FINR (Switzerland) & EBIR
Endovascular Surgeon & Consultant Interventional Neuroradiologist at Care CHL Hospital, Indore Co-director CVIC( center for vascular and interventional care)
DR. NISHANT BHARGAVA
Consultant Intervention Radiologist
MD Radiology, PDCC ( Neurointervention Radiology), FINR ( Fellowship in Neurointervention Radiology)
Co-director CVIC(Center for Vascular and Interventional Care)
Contact Details
Phone no.
0731 4675670
+91 9827760073
Facebook
https://www.facebook.com/profile.php?id=100092538633553&mibextid=ZbWKwL
Instagram
https://instagram.com/cvic_center?igshid=ZGUzMzM3NWJiOQ==
Google My business
https://g.co/kgs/DrdV3T
YouTube
https://www.youtube.com/channel/UCP5TH5e4iQZkpDUgnLsgZhw
Pinterest
https://pin.it/5DzpX5Z
Twitter
https://x.com/cviccenter?t=01TclSrLFdu0K2re0Gs96w&s=08
LINKEDIN
https://www.linkedin.com/company/center-of-vascular-interventional-care/
Location –
Read More –
How much does AVM embolization cost? – https://cvicvascular.com/avm-embolization-cost/
10 Essential Insights into the Indications and Problems of Intracranial Stenting – https://cvicvascular.com/indications-and-problems-of-intracranial-stenting/
Conquering Spinal AVMs: The Power of Embolization – https://cvicvascular.com/spinal-avm-embolization/