What is a PCN Procedure in Urology?
Urology, a branch of medicine that focuses on the urinary tracts of males and females, and the reproductive system of males, often requires precise interventions to address complex conditions. One such intervention is the Percutaneous Nephrostomy (PCN), which is vital for patients with certain urinary tract issues. This detailed article delves into what a PCN Procedure in Urology, its applications, the preparation involved, potential risks, and the recovery process, providing a comprehensive understanding of this medical procedure.
Introduction to PCN in Urology
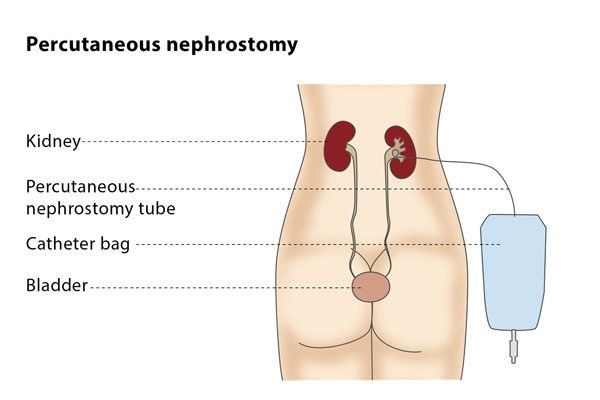
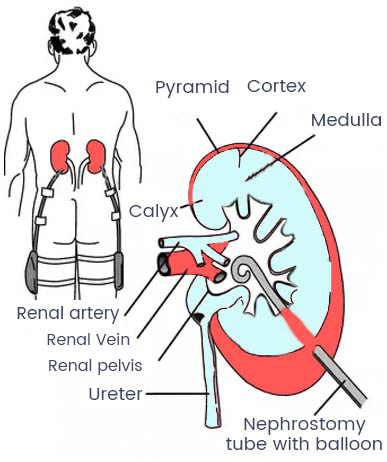
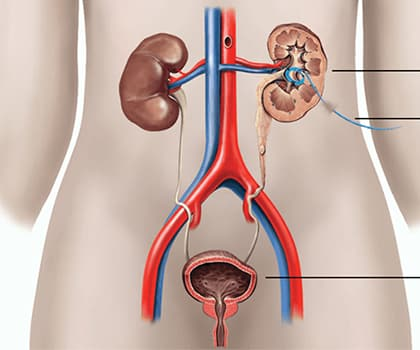
Percutaneous Nephrostomy (PCN) is a specialized medical procedure employed by urologists to ensure urine flow from the kidneys when normal flow is blocked. Blocks can arise due to various conditions such as kidney stones, tumors, or strictures in the ureter. PCN involves the insertion of a catheter directly into the kidney through the skin, bypassing any obstructions in the urinary tract. This procedure not only alleviates symptoms but also prevents further complications, such as kidney damage.
Understanding the Need for PCN
Indications for PCN
A Percutaneous Nephrostomy (PCN) is an essential medical procedure in the field of urology that is primarily indicated for relieving an obstruction in the urinary tract when less invasive treatments are ineffective or inappropriate. The procedure involves inserting a catheter directly into the kidney to bypass blockages in the urinary system, allowing for the drainage of urine directly from the kidney to the outside of the body. Here are some of the key indications for a PCN procedure:
Severe Urinary Tract Obstructions
The most common and critical indication for a PCN is an obstruction in the urinary tract that poses an immediate threat to kidney function. This can be due to a variety of causes:
- Kidney Stones: Large stones that are unable to pass through the urinary tract and cause severe pain or infection may necessitate a PCN, especially if they block urine flow to a significant extent.
- Ureteropelvic Junction (UPJ) Obstruction: This condition involves a blockage at the junction where the ureter joins the kidney, which can be congenital or acquired.
- Ureteral Strictures: Narrowing of the ureters due to injury, surgery, or disease can lead to significant obstruction, requiring intervention like PCN.
Support for Other Urological Procedures
PCN can also be used as a preparatory or adjunct procedure in various urological interventions:
- Before Ureteroscopy or Lithotripsy: To decompress the renal system and facilitate the passage of instruments or shock waves for stone fragmentation.
- Post-surgical Complications: After surgeries like kidney transplants or tumor removals, if there is a risk of urine leakage or if the normal urinary pathway needs time to heal, a PCN might be employed.
Tumors Causing Obstructions
Tumors within the kidney or those impinging on the urinary tract can lead to blockages. PCN provides a way to manage kidney function while awaiting more definitive treatment such as surgery, chemotherapy, or radiation:
- Renal or Ureteral Tumors: Malignant or benign growths can obstruct the flow of urine, necessitating a PCN.
- Extrinsic Compression: Tumors in nearby organs (like ovarian or cervical cancer) can press on the ureters, blocking urine flow.
Infections and Inflammatory Conditions
In certain cases, infections or inflammation can lead to severe swelling, which in turn obstructs urine flow. PCN is used to manage such conditions:
- Pyonephrosis: This is an infection of the kidney that leads to the accumulation of pus under pressure, which can be life-threatening if not drained.
- Xanthogranulomatous Pyelonephritis (XGP): A severe, chronic infection that leads to the destruction of the renal parenchyma, often requiring both antibiotic therapy and drainage.
Palliative Care
In patients with advanced malignancies or other chronic conditions where surgical intervention is not feasible or desirable, PCN can provide significant symptomatic relief from the pain and discomfort caused by urinary obstructions.
Benefits of PCN
Percutaneous Nephrostomy (PCN) is an invaluable procedure in urology, offering numerous benefits especially for patients experiencing obstructive uropathy where traditional pathways for urine flow are compromised. This intervention not only serves as an emergency relief but also as a strategic approach in the management of various urinary tract conditions. Here’s a closer look at the multiple benefits of undergoing a PCN procedure:
Immediate Relief from Symptoms
The primary benefit of PCN is the rapid alleviation of symptoms associated with urinary tract obstructions, such as:
- Pain Relief: Urinary obstructions often cause severe flank pain due to increased pressure in the kidney. PCN immediately reduces this pressure, significantly easing pain.
- Reduction in Infection Risk: By enabling the drainage of urine, PCN helps flush out bacteria from the urinary system, thereby reducing the risk of infections like pyelonephritis or sepsis, which can occur due to stagnant urine.
Prevention of Further Complications
A PCN can prevent several serious health complications associated with obstructed urine flow:
- Prevention of Kidney Damage: Chronic obstruction can lead to hydronephrosis, which can impair kidney function and eventually lead to renal failure if not promptly managed. PCN mitigates this risk by ensuring continued urine flow.
- Preservation of Renal Function: In cases of bilateral obstructions or in single functioning kidneys, maintaining urine flow is crucial for preserving kidney health and function. PCN provides a reliable pathway for urine, safeguarding renal function.
Facilitates Other Medical Procedures
PCN is not only beneficial as a standalone procedure but also supports other medical interventions:
- Diagnostic Clarity
- Preoperative and Postoperative Support
Long-Term Management Option
For patients who cannot undergo surgery due to medical reasons or where surgery has failed, PCN provides a viable long-term solution:
- Chronic Conditions: In patients with chronic conditions such as recurrent stones or malignancies that repeatedly cause blockages, PCN can serve as a long-term management strategy to maintain quality of life.
- Palliative Care: In terminal illnesses where curative treatment is no longer an option, PCN can be used to provide comfort by relieving the symptoms of urinary obstruction.
Enhanced Quality of Life
By managing the physical symptoms effectively, PCN significantly enhances the patient’s quality of life:
- Symptom Management: Effective control of pain and urinary symptoms allows patients to return to their daily activities sooner and with greater comfort.
- Psychological Relief: Reducing the physical discomfort associated with urinary tract issues also helps alleviate the anxiety and stress that often accompany these conditions.
Flexibility and Safety
The PCN procedure is known for its flexibility and safety profile:
- Minimally Invasive: Being a minimally invasive procedure, PCN involves less risk than traditional open surgery and typically has a faster recovery time.
- Controlled and Monitored: The procedure is performed under imaging guidance, which minimizes risks and improves the accuracy of the catheter placement.
In summary, the PCN procedure provides essential benefits, from immediate symptom relief to long-term management of urinary tract conditions. Its role in preventing complications, supporting other medical treatments, and enhancing the overall quality of life makes it a critical option in contemporary urological practice. By ensuring ongoing kidney function and managing complications associated with urinary tract obstructions, PCN plays a pivotal role in both acute and chronic urological care settings.
Preparing for a PCN Procedure
Pre-Procedure Assessments
Before a PCN procedure, thorough diagnostic assessments are crucial to determine the exact cause and location of the obstruction. These typically include:
- Ultrasound to visualize the kidneys and surrounding tissues.
- CT scans for a more detailed view of the urinary tract.
- Blood tests to assess kidney function and overall health.
Patient Preparation Guidelines
Patients scheduled for a PCN procedure need to follow specific guidelines to ensure the safety and success of the procedure:
- Fasting for a certain period before the procedure.
- Adjusting medications, especially blood thinners, under medical advice.
- Arranging for someone to drive home post-procedure due to the effects of sedation.
The PCN Procedure: A Step-by-Step Overview
Performing the Procedure
The PCN procedure is typically performed under local anesthesia and sedation, ensuring the patient remains comfortable. The steps include:
- The patient is positioned to expose the back where the kidneys are accessible.
- The skin is sterilized and a local anesthetic is applied.
- Using ultrasound or fluoroscopic guidance, a needle is carefully inserted through the skin into the kidney.
- A guide wire is passed through the needle, and a catheter is placed over the wire into the kidney to ensure urine can bypass any obstructions.
Post-Procedure Monitoring
After the PCN tube is successfully placed, patients are monitored for any immediate complications, such as bleeding or infection. Monitoring includes:
- Regular checks on vital signs.
- Assessment of the catheter site for any signs of infection.
- Ultrasound to ensure the catheter is properly positioned.
Risks and Complications of PCN
No medical procedure is without risks. For PCN, potential complications may include:
- Bleeding around the kidney or along the path of the catheter.
- Infection at the catheter insertion site or within the kidney.
- Accidental dislodgment of the catheter.
- Rarely, injury to surrounding organs such as the liver, spleen, or lungs.
Recovery and Aftercare Following a PCN Procedure
Immediate Post-Procedure Care
Immediately following the procedure, patients might experience some discomfort, which can generally be managed with pain medication. It’s crucial to monitor the catheter output and ensure the
catheter remains secure. Instructions on catheter care and signs of complications will be provided before discharge.
Long-Term Management
For patients with a long-term PCN catheter, ongoing care is essential to prevent complications. This includes regular catheter changes, monitoring for signs of infection, and ensuring the catheter is functioning properly. Patients will also have regular follow-ups to assess the need for continued PCN or other interventions.
Conclusion: The Significance of PCN in Urology
The PCN procedure is a testament to the advancements in medical technology and technique, providing a lifeline for patients with severe urinary tract obstructions. By understanding the nuances of this procedure, patients and their families can make informed decisions and prepare adequately for both the procedure and the recovery phase. With proper management, PCN can significantly improve quality of life and prevent serious kidney-related health issues.
FAQs
What is a PCN procedure used for in urology?
A PCN procedure, or percutaneous nephrostomy, is primarily used to relieve obstruction in the urinary tract that threatens kidney function, caused by conditions like stones, tumors, or strictures.
How is the PCN procedure performed?
The procedure involves inserting a catheter directly into the kidney through the skin under local anesthesia and sedation, guided by ultrasound or fluoroscopy to bypass the obstruction in the urinary tract.
What are the risks associated with a PCN procedure?
Risks include bleeding, infection, accidental dislodgment of the catheter, and rarely, injury to surrounding organs.
How long does recovery from a PCN procedure take?
Recovery varies depending on the individual’s health and the complexity of the procedure. Most patients can resume normal activities within a few days but may require ongoing catheter care if the catheter remains in place longer.
Can a PCN catheter be a long-term solution?
Yes, a PCN catheter can be used as a long-term solution in cases where surgical removal of obstructions is not possible or advisable. Regular monitoring and catheter changes are necessary to prevent complications.
Our Doctors
Dedicated IR Center for Vascular Problems in Madhya Pradesh
DR. SHAILESH GUPTA
MD, PDCC (INTERVENTIONAL RADIOLOGY) Consultant & Co-Director CVIC (Center Of Vascular & Interventional Care)
DR. ALOK KUMAR UDIYA
MD Radiology, PDCC (Neurointervention Radiology), PDCC ( HPB Intervention Radiology) FINR (Switzerland) & EBIR
Endovascular Surgeon & Consultant Interventional Neuroradiologist at Care CHL Hospital, Indore Co-director CVIC( center for vascular and interventional care)https://interventionradiologyindore.com/
DR. NISHANT BHARGAVA
Consultant Intervention Radiologist
MD Radiology, PDCC ( Neurointervention Radiology), FINR ( Fellowship in Neurointervention Radiology)
Co-director CVIC(Center for Vascular and Interventional Care)
Contact Details
Phone no.
0731 4675670
+91 9827760073
Facebook
https://www.facebook.com/profile.php?id=100092538633553&mibextid=ZbWKwL
Instagram
https://instagram.com/cvic_center?igshid=ZGUzMzM3NWJiOQ==
Google My business
https://g.co/kgs/DrdV3T
YouTube
https://www.youtube.com/channel/UCP5TH5e4iQZkpDUgnLsgZhw
Pinterest
https://pin.it/5DzpX5Z
Twitter
https://x.com/cviccenter?t=01TclSrLFdu0K2re0Gs96w&s=08
LINKEDIN
https://www.linkedin.com/company/center-of-vascular-interventional-care/
Location
PCN Procedure in Urology
Read More –
Thrombolysis: Definition, Types, Uses, Effects, and More – https://cvicvascular.com/thrombolysis/
Navigating Cancer Treatment: Understanding Transarterial Chemoembolization (TACE) – https://cvicvascular.com/navigating-cancer-treatment-tace/
Life expectancy after a liver TIPS procedure – https://cvicvascular.com/life-expectancy-after-liver-tips-procedure/