PTBD and Stenting for Malignant Obstructive Jaundice
When it comes to managing malignant obstructive jaundice, percutaneous transhepatic biliary drainage (PTBD) and stenting stand out as pivotal medical interventions. These procedures not only alleviate the symptoms caused by bile duct obstructions but also significantly improve the quality of life for patients suffering from advanced cancers. This detailed guide delves into the nuances of PTBD and stenting, providing a comprehensive look at how these procedures are performed, their benefits, potential risks, and what patients can expect during recovery.
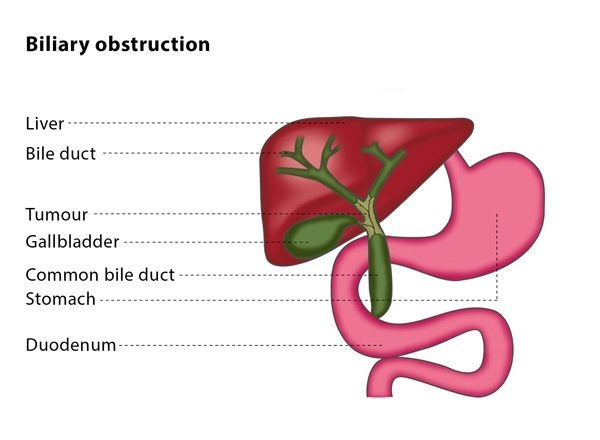
Understanding Malignant Obstructive Jaundice
Obstructive jaundice is a medical condition characterized by the yellowing of the skin and eyes, which occurs when there is a blockage in the bile duct system preventing bile from reaching the intestines. This section delves into the fundamentals of obstructive jaundice, exploring its causes, symptoms, and implications for overall health.
What Causes Obstructive Jaundice?
Obstructive jaundice is typically caused by conditions that block the bile ducts. These obstructions can be due to various factors including:
- Gallstones: The most common cause, where stones formed in the gallbladder block the bile ducts.
- Tumors: Malignancies such as pancreatic cancer, liver cancer, or bile duct cancer can compress or invade the bile ducts.
- Pancreatitis: Inflammation of the pancreas can lead to swelling and blockage of the bile duct.
- Biliary Strictures: Narrowing of the bile ducts due to injury, surgery, or disease can restrict bile flow.
Symptoms of Obstructive Jaundice
The symptoms of obstructive jaundice can vary depending on the underlying cause and severity of the blockage. Common symptoms include:
- Jaundice: Yellowing of the skin and the whites of the eyes, which is the most noticeable symptom.
- Dark Urine: Caused by excess bilirubin being excreted through the kidneys.
- Pale Stools: Lack of bile in the intestines can cause stools to be light-colored or clay-colored.
- Itching: Accumulation of bile salts in the skin can lead to severe itching.
- Abdominal Pain: Especially in the upper right quadrant, which can be a sign of gallstones or tumors.
- Weight Loss and Fever: These may accompany jaundice if the cause is related to infection or malignancy.
Diagnosing Obstructive Jaundice
Diagnosis of obstructive jaundice typically involves a combination of clinical evaluation and diagnostic tests, including:
- Blood Tests: To measure levels of bilirubin, liver enzymes, and other substances that indicate liver function.
- Imaging Tests: Ultrasound, CT scan, and MRI can provide detailed images of the bile ducts, gallbladder, and liver to identify blockages.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): A specialized procedure used not only to diagnose but also to treat obstructions in the bile ducts.
Complications of Obstructive Jaundice
If left untreated, obstructive jaundice can lead to several serious complications such as:
- Cholangitis: An infection of the bile ducts, which can be life-threatening if not treated promptly.
- Liver Damage: Prolonged bile obstruction can lead to liver dysfunction and eventually liver failure.
- Biliary Cirrhosis: Scarring of the bile ducts, which can impair liver function over time.
Management and Treatment
The treatment for obstructive jaundice focuses on resolving the bile duct obstruction. Treatment options include:
- Surgical Removal: Removing gallstones or tumors that are causing the blockage.
- Endoscopic Stenting: Placing a stent to keep the bile duct open.
- Percutaneous Drainage: In cases where endoscopic treatment is not possible, an external drain may be placed to bypass the blockage.
Understanding the basics of obstructive jaundice is crucial for recognizing its signs and symptoms, pursuing timely diagnosis, and effectively managing the condition to prevent severe complications.
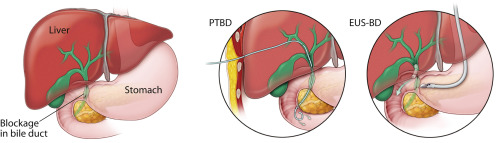
What is Percutaneous Transhepatic Biliary Drainage?
Percutaneous Transhepatic Biliary Drainage (PTBD) is a medical procedure used to relieve obstruction of the bile ducts, which is often caused by tumors, strictures, or stones that block the normal flow of bile from the liver to the intestines. This technique is particularly valuable when endoscopic methods are not feasible or have been unsuccessful. Here, we’ll explore how PTBD is performed, its indications, and the role it plays in the management of biliary obstructions.
Procedure Explained
PTBD is performed under image guidance, typically using ultrasound and fluoroscopy, to ensure accuracy in catheter placement. The process involves several key steps:
- Local Anesthesia and Sedation: The patient is usually given local anesthesia and sedative medications to minimize discomfort during the procedure.
- Needle Insertion: A radiologist inserts a thin needle through the skin (percutaneously) into the liver, targeting the bile ducts.
- Catheter Placement: Once the bile ducts are accessed, a catheter is threaded through the needle to provide a pathway for bile to drain externally or internally, depending on the patient’s needs.
- Bile Drainage: The bile is either diverted externally into a collecting bag or internally by placing a stent that bypasses the obstruction, allowing bile to flow directly into the small intestine.
Indications for PTBD
PTBD is considered in several scenarios where biliary decompression is necessary, including:
- Malignant Obstructions: Commonly in cases of pancreatic cancer, liver cancer, or cancers of the gallbladder and bile ducts that compress or invade the bile ducts.
- Benign Conditions: Such as biliary strictures or stones that cannot be removed endoscopically.
- Pre-operative Cases: To reduce jaundice levels before surgery in patients undergoing liver surgery or transplantation.
- Post-operative Complications: To manage biliary leaks or other complications following abdominal surgery.
Benefits of PTBD
The benefits of PTBD are significant, especially for patients who cannot undergo surgery or more invasive procedures:
- Effective Biliary Drainage: PTBD provides a direct method to relieve jaundice and reduce bilirubin levels, alleviating symptoms and improving liver function.
- Minimally Invasive: As a less invasive alternative to surgery, PTBD typically results in shorter recovery times and reduced hospital stays.
- Palliative Care: In patients with advanced cancer, PTBD can significantly improve quality of life by reducing symptoms related to biliary obstruction.
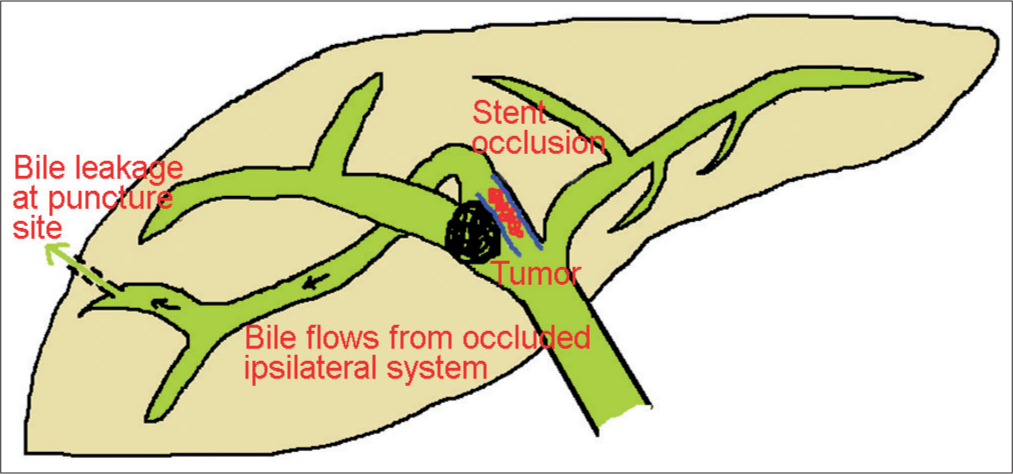
Risks and Considerations
While PTBD is a valuable procedure, it comes with potential risks that must be considered:
- Infection: The most common complication, which can generally be managed with antibiotics.
- Bleeding: There is a risk of bleeding from liver puncture, although severe cases are rare.
- Biliary Peritonitis: If bile leaks into the abdominal cavity, it can lead to inflammation, requiring prompt medical attention.
Post-Procedure Care
After PTBD, patients typically need to stay in the hospital for a few days to ensure the catheter is functioning properly and to manage any immediate complications. Regular follow-up appointments are crucial to monitor the site of catheter insertion and the overall function of the bile drainage system. Adjustments to the catheter or additional interventions may be necessary depending on the patient’s response to the procedure and progression of the underlying disease.
In conclusion, PTBD is a critical procedure in the management of biliary obstructions, particularly when less invasive endoscopic methods are not an option. Its ability to relieve symptoms, improve liver function, and enhance quality of life makes it a valuable tool in the treatment of both malignant and benign biliary conditions.
The Role of Stenting in Managing Biliary Obstructions
Stenting plays a crucial role in the management of biliary obstructions, particularly those caused by tumors, strictures, or other blockages that impair the normal flow of bile from the liver to the intestines. Biliary stents are devices designed to open up blocked ducts and maintain the patency of the bile ducts, ensuring that bile can flow freely. This section explores the various types of biliary stents, their benefits, and the clinical scenarios where they are most effectively employed.
Types of Biliary Stents
Biliary stents come in different materials and designs, each suited to specific types of obstructions and expected duration of use:
- Plastic Stents: These are commonly used for temporary relief in cases where short-term stenting is anticipated. Plastic stents are less expensive but may need to be replaced every few months because they can become clogged over time.
- Metal Stents: Made from materials like nitinol or stainless steel, metal stents are more durable and are generally used when long-term stenting is required. They expand to a larger diameter than plastic stents, providing better drainage and a lower risk of occlusion. Metal stents are particularly useful in malignant cases where tumor growth may compress the ducts.
- Covered Metal Stents: These stents have a coating that reduces the risk of the stent being invaded by tumor cells or becoming occluded by tissue ingrowth. They are often used in malignant conditions to extend the functional life of the stent.
Benefits of Biliary Stenting
The insertion of biliary stents offers several key benefits:
- Relief of Symptoms: Stenting effectively alleviates symptoms of jaundice, including severe itching, yellowing of the skin and eyes, and dark urine, thus improving the patient’s quality of life.
- Improved Liver Function: By restoring bile flow, stenting helps normalize liver function tests and reduces the risk of liver damage and biliary cirrhosis.
- Enables Other Treatments: For cancer patients, relieving the jaundice can make them better candidates for chemotherapy or radiation therapy, as it improves liver function and overall health.
- Palliative Care: In cases of inoperable tumors, stenting provides a palliative approach to manage symptoms and improve comfort without curative intent.
Procedure for Placing a Biliary Stent
The placement of a biliary stent typically involves an endoscopic or percutaneous approach, depending on the location of the obstruction and the patient’s overall condition:
- Endoscopic Retrograde Cholangiopancreatography (ERCP): This is the most common method for stent placement. A flexible tube with a camera (endoscope) is inserted through the mouth, down the stomach, and into the duodenum where the bile ducts empty. Tools can be passed through the endoscope to place the stent directly into the bile duct.
- Percutaneous Transhepatic Biliary Drainage (PTBD): If ERCP is not possible, PTBD may be used as an alternative. This involves inserting a stent through the skin (percutaneously) with the guidance of imaging technology.
Risks and Complications
Like any medical procedure, the placement of biliary stents carries some risks:
- Infection: There is a risk of infection both from the procedure itself and from the stent.
- Stent Migration: The stent may move from its original position, which can lead to ineffective drainage or damage to the bile duct.
- Stent Occlusion: Over time, stents can become blocked by sludge, tumor growth, or bile crystals, requiring replacement or additional procedures.
Follow-Up Care
Regular monitoring and follow-up are essential to ensure the continued effectiveness of the stent and to manage any complications promptly.
In conclusion, the role of stenting in managing biliary obstructions is indispensable, particularly in complex or malignant cases. By alleviating symptoms and restoring bile flow, stenting significantly enhances patient outcomes and quality of life.
Procedure Preparation and Execution
Preparing for PTBD and Stenting
Proper preparation is essential for the success of PTBD and stenting. This section covers the necessary pre-procedure steps, including fasting, medication adjustments, and what patients should bring on the day of the procedure.
During the Procedure: What to Expect
For many patients, knowing what happens during the procedure can reduce anxiety. This detailed description provides insight into what occurs during PTBD and stenting, from start to finish.
Post-Procedure Care and Recovery
Immediate Post-Procedure Care
Immediate care following PTBD and stenting is critical. This subsection describes the initial recovery period, monitoring, and management of any immediate post-procedure symptoms.
Long-Term Management and Follow-up
Sustained recovery and monitoring are vital for ensuring the long-term success of the treatment. This part discusses the follow-up schedule, lifestyle adjustments, and long-term complications to watch for.
Potential Complications and Risks
Recognizing and Managing Complications
While PTBD and stenting are generally safe, they carry risks of complications such as infections, bleeding, and stent blockage.
When to Seek Emergency Care
This section outlines the warning signs that indicate a need for urgent medical attention, ensuring that patients and caregivers can react swiftly to any adverse developments.
Patient Stories and Outcomes
Real-Life Experiences
Sharing patient stories can be incredibly empowering and informative. This subsection includes testimonials from individuals who have undergone PTBD and stenting, providing diverse perspectives on the procedures.
Statistical Success Rates
To provide a broader view of the procedures’ effectiveness, this part presents statistical data on success rates and patient outcomes post-PTBD and stenting.
Conclusion
Percutaneous transhepatic biliary drainage and stenting are vital procedures for managing malignant obstructive jaundice. By understanding the procedure, preparing adequately, and managing recovery, patients can achieve significant relief and a better quality of life.
FAQs
- What should I expect during recovery from PTBD and stenting?
- How often will I need follow-up visits after the procedure?
- What are the signs of complications I should be aware of after PTBD?
- What lifestyle changes can help me manage my condition post-procedure?
- How effective is PTBD and stenting in alleviating malignant obstructive jaundice?
The journey through PTBD and stenting for malignant obstructive jaundice involves a thorough understanding of the procedures, adequate preparation, and diligent post-procedure care. With the right approach, patients can navigate their treatment with confidence and improve their overall well-being.
Our Doctors
Dedicated IR Center for Vascular Problems in Madhya Pradesh
DR. SHAILESH GUPTA
MD, PDCC (INTERVENTIONAL RADIOLOGY) Consultant & Co-Director CVIC (Center Of Vascular & Interventional Care)
DR. ALOK KUMAR UDIYA
MD Radiology, PDCC (Neuro intervention Radiology), PDCC ( HPB Intervention Radiology) FINR (Switzerland) & EBIR
Endovascular Surgeon & Consultant Interventional Neuroradiologist at Care CHL Hospital, Indore Co-director CVIC( center for vascular and interventional care) https://interventionradiologyindore.com/
DR. NISHANT BHARGAVA
Consultant Intervention Radiologist
MD Radiology, PDCC ( Neuro intervention Radiology), FINR ( Fellowship in Neuro intervention Radiology)
Co-director CVIC(Center for Vascular and Interventional Care)
Contact Details
Phone no.
0731 4675670
+91 9827760073
Facebook
https://www.facebook.com/profile.php?id=100092538633553&mibextid=ZbWKwL
Instagram
https://instagram.com/cvic_center?igshid=ZGUzMzM3NWJiOQ==
Google My business
https://g.co/kgs/DrdV3T
YouTube
https://www.youtube.com/channel/UCP5TH5e4iQZkpDUgnLsgZhw
Pinterest
https://pin.it/5DzpX5Z
Twitter
https://x.com/cviccenter?t=01TclSrLFdu0K2re0Gs96w&s=08
LINKEDIN
https://www.linkedin.com/company/center-of-vascular-interventional-care/
Location
PTBD and Stenting for Malignant Obstructive Jaundice
Read More –
Targeted Victory: Mastering Chemo Embolization in Cancer Treatment – https://cvicvascular.com/targeted-victory-mastering-chemo-embolization-in-cancer-treatment/
Understanding Chemotherapy Ports: A Guide to Easier and Safer Cancer Treatment – https://cvicvascular.com/chemotherapy-port-insertion/
Streamlining Care: Navigating the Essentials of PICC Line Placement – https://cvicvascular.com/streamlining-care-navigating-the-essentials-of-picc-line-placement/