Introduction
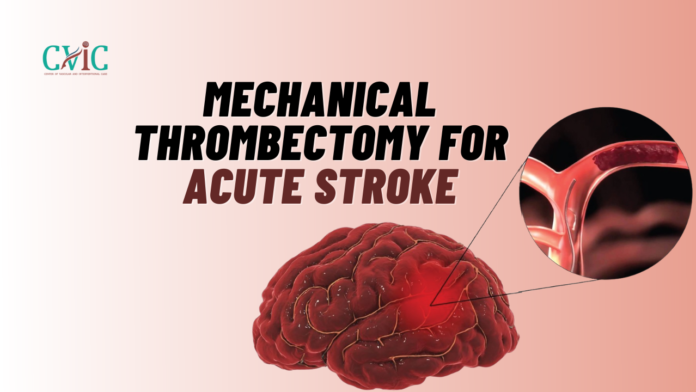
Every second counts when it comes to treating acute strokes, a medical emergency that can have devastating consequences. Time-sensitive interventions are crucial to minimize brain damage and improve outcomes for stroke patients. In recent years, a ground breaking procedure known as Mechanical Thrombectomy has emerged as a game-changer in the field of stroke treatment. In this comprehensive blog, we will explore the intricacies of Mechanical Thrombectomy for Acute Stroke, its history, procedure, efficacy, and impact on the landscape of acute stroke care.
Understanding Acute Strokes
Before delving into the specifics of Mechanical Thrombectomy, it is essential to grasp the fundamentals of acute strokes. Strokes occur when blood flow to a part of the brain is disrupted, either due to a blockage (ischemic stroke) or bleeding (hemorrhagic stroke). Ischemic strokes, which account for the majority of cases, often result from the formation of blood clots that obstruct blood vessels in the brain.
Evolution of Stroke Treatment
Traditionally, the standard of care for ischemic strokes involved the administration of tissue plasminogen activator (tPA), a clot-busting drug. While tPA has proven effective when administered within a narrow time window, its efficacy diminishes as time elapses. Furthermore, not all patients are eligible for tPA, underscoring the need for alternative interventions.
Enter Mechanical Thrombectomy
Historical Context
Mechanical Thrombectomy is not a recent innovation; its roots can be traced back to the early attempts at removing blood clots from cerebral vessels. However, it gained prominence in the 2010s with advancements in medical technology and imaging techniques.
How It Works
Mechanical Thrombectomy involves the use of a catheter-based procedure to physically remove blood clots from the brain’s blood vessels. Guided by real-time imaging, a catheter is threaded through the blood vessels to the site of the clot. Once the catheter reaches the clot, a stent retriever or similar device is deployed to ensnare and extract the obstruction.
The Procedure Unveiled
Patient Selection
Not every stroke patient is a candidate for Mechanical Thrombectomy. Selection criteria include the location and size of the clot, the time elapsed since the onset of symptoms, and the patient’s overall health. Rapid and accurate diagnosis is pivotal in determining eligibility for this intervention.
Imaging Techniques
Advanced imaging modalities, such as computed tomography angiography (CTA) and magnetic resonance imaging (MRI), play a crucial role in identifying eligible patients and guiding the intervention. These techniques provide detailed images of the cerebral vasculature, aiding in the precise localization of clots.
The Time Factor
Time is of the essence in stroke care, and the effectiveness of Mechanical Thrombectomy is highly time-dependent. The procedure is most beneficial when performed within a specific time window from the onset of symptoms, emphasizing the need for streamlined processes and rapid response systems.
Efficacy and Outcomes
Clinical Trials
The efficacy of Mechanical Thrombectomy has been rigorously evaluated in numerous clinical trials, including landmark studies like MR CLEAN, ESCAPE, and REVASCAT. These trials consistently demonstrated the superiority of Mechanical Thrombectomy over standard medical therapy alone in improving functional outcomes for stroke patients.
Improved Functional Independence
One of the most compelling outcomes of Mechanical Thrombectomy is its ability to significantly improve functional independence in stroke survivors. By swiftly restoring blood flow to the affected brain regions, the procedure minimizes neurological deficits and enhances the chances of a full recovery.
Safety Considerations
While Mechanical Thrombectomy is generally well-tolerated, like any medical procedure, it carries some risks. Complications may include vessel injury, bleeding, or embolization of clot fragments to other parts of the brain. However, the overall safety profile is favorable when weighed against the potential benefits.
Impact on Stroke Care Landscape
Changing Treatment Paradigms
The advent of Mechanical Thrombectomy has transformed the landscape of acute stroke care. It has prompted a paradigm shift, with an increasing emphasis on endovascular interventions and the establishment of comprehensive stroke centers equipped with the necessary expertise and infrastructure.
Telestroke Services
Recognizing the time-sensitive nature of stroke care, telestroke services have become integral in facilitating timely access to Mechanical Thrombectomy. Through telemedicine, stroke specialists can remotely assess patients, review imaging studies, and make rapid decisions regarding the appropriateness of intervention.
Challenges and Future Directions
Access Disparities
Despite its efficacy, challenges exist in ensuring equitable access to Mechanical Thrombectomy. Disparities in geographical distribution, healthcare infrastructure, and awareness can hinder timely access for certain populations.
Expanding Treatment Windows
Ongoing research is focused on expanding the treatment window for Mechanical Thrombectomy, allowing more patients to benefit from this intervention. Innovations in imaging technology and a deeper understanding of the biological underpinnings of stroke may contribute to extending the therapeutic time frame.
Combining Therapies
The future of stroke treatment may involve a multimodal approach, combining Mechanical Thrombectomy with pharmacological agents or neuroprotective strategies to further enhance outcomes and minimize complications.
Conclusion
In conclusion, Mechanical Thrombectomy represents a revolutionary advancement in the treatment of acute ischemic strokes. Its ability to swiftly restore blood flow to the brain, coupled with the evidence from rigorous clinical trials, has established it as a cornerstone in the modern approach to stroke care. As research and technological innovations continue, the future holds promise for further refining and expanding the scope of Mechanical Thrombectomy, ultimately improving the lives of countless individuals affected by acute strokes.
Our Doctors
Dedicated IR Center for Vascular Problems in Madhya Pradesh
DR. SHAILESH GUPTA
MD, PDCC (INTERVENTIONAL RADIOLOGY) Consultant & Co-Director CVIC (Center Of Vascular & Interventional Care)
DR. ALOK KUMAR UDIYA
MD Radiology, PDCC (Neurointervention Radiology), PDCC ( HPB Intervention Radiology) FINR (Switzerland) & EBIR
Endovascular Surgeon & Consultant Interventional Neuroradiologist at Care CHL Hospital, Indore Co-director CVIC( center for vascular and interventional care)
DR. NISHANT BHARGAVA
Consultant Intervention Radiologist
MD Radiology, PDCC ( Neurointervention Radiology), FINR ( Fellowship in Neurointervention Radiology)
Co-director CVIC(Center for Vascular and Interventional Care)
Contact Details
Phone no.
0731 4675670
+91 9827760073
Facebook
https://www.facebook.com/profile.php?id=100092538633553&mibextid=ZbWKwL
Instagram
https://instagram.com/cvic_center?igshid=ZGUzMzM3NWJiOQ==
Google My business
https://g.co/kgs/DrdV3T
YouTube
https://www.youtube.com/channel/UCP5TH5e4iQZkpDUgnLsgZhw
Pinterest
https://pin.it/5DzpX5Z
Twitter
https://x.com/cviccenter?t=01TclSrLFdu0K2re0Gs96w&s=08
LINKEDIN
https://www.linkedin.com/company/center-of-vascular-interventional-care/
Location –
Read More –
Pre-Operative Embolization of Tumors: A Lifesaving Strategy – https://cvicvascular.com/pre-operative-embolization-of-tumors-a-lifesaving-strategy/
AVM Embolization: A Comprehensive Guide to the Procedure – https://cvicvascular.com/avm-embolization-a-comprehensive-guide-to-the-procedure/
Intracranial Stenting: A Comprehensive Guide – https://cvicvascular.com/intracranial-stenting-a-comprehensive-guide/