Is It Normal to Bleed After Embolization?
Experiencing bleeding after embolization can be concerning for many patients. This procedure, often used to treat various medical conditions by blocking blood vessels, has its set of post-operative expectations and potential complications. Understanding whether bleeding is a normal part of the recovery process is crucial for effective post-procedure care and stress alleviation.
Introduction to Embolization
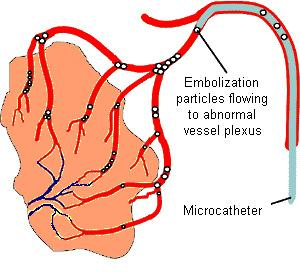
Embolization is a therapeutic medical procedure used to deliberately block a blood vessel to prevent blood flow to a specific area of the body. This technique is commonly employed to treat a variety of conditions such as arteriovenous malformations, gastrointestinal bleeding, and certain types of tumors. By understanding the procedure, patients can better prepare for what to expect during and after embolization, including potential bleeding.
What Is Embolization Used For?
The Scope and Utility of Embolization
Embolization serves a critical role in managing various medical conditions. It is particularly beneficial in situations where surgery poses too high a risk or when less invasive measures are preferred. This section will delve into the specific conditions that embolization can effectively treat.
Embolization is a specialized medical procedure that involves the intentional blocking of one or more blood vessels to prevent blood flow to a specific area of the body. This technique is utilized across a broad spectrum of medical disciplines and for various health conditions, demonstrating its versatility and critical utility in contemporary medicine. The scope of embolization is vast, covering treatment from non-malignant conditions to life-threatening emergencies.
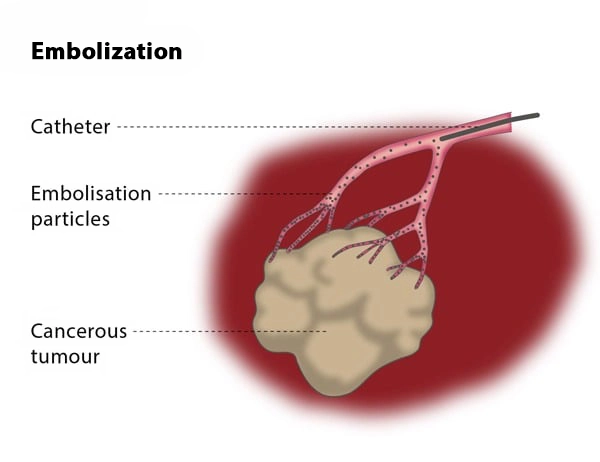
Applications in Treating Tumors
One of the primary applications of embolization is in the treatment of tumors, including those in the liver, kidneys, and lungs. For example, in liver cancer, embolization can be used to block the blood supply to a tumor, effectively starving it of the necessary nutrients and oxygen required for its growth. This method, known as transarterial chemoembolization (TACE), combines embolization with localized chemotherapy, thereby maximizing the therapeutic effect while minimizing systemic side effects.
Managing Vascular Anomalies
Embolization is pivotal in the management of vascular anomalies such as arteriovenous malformations (AVMs) and aneurysms. AVMs are abnormal connections between arteries and veins that disrupt normal blood flow and oxygen circulation. Embolization helps by reducing the risk of bleeding and subsequent complications such as strokes or brain damage. In the case of aneurysms, particularly those that are inoperable, embolization can prevent rupture by filling the aneurysm sac with materials that promote blood clotting and vessel sealing.
Control of Hemorrhagic Conditions
For patients experiencing severe bleeding (hemorrhage), whether due to trauma, surgical complications, or inherent bleeding disorders, embolization offers a rapid and effective means to control life-threatening situations without the need for extensive surgery. This application is frequently seen in conditions like gastrointestinal bleeding, where direct embolization of the bleeding vessel can promptly stop the hemorrhage, thereby stabilizing the patient’s condition quickly.
Benefits in Gynecology
In gynecology, embolization has a significant role, particularly in the management of uterine fibroids, benign tumors of the uterus that can cause heavy menstrual bleeding, pain, and other reproductive complications. Uterine artery embolization (UAE) offers a less invasive alternative to hysterectomy and myomectomy, with fewer complications and a shorter recovery period, making it a preferred option for many women.
Prostatic Artery Embolization
Recently, the scope of embolization has expanded to include prostatic artery embolization for the treatment of benign prostatic hyperplasia (BPH), a common condition in older men characterized by the enlargement of the prostate gland. This procedure has shown promising results in reducing prostate size and alleviating symptoms without the risks associated with traditional surgical procedures such as resection of the prostate.
Minimally Invasive Nature and Reduced Recovery Time
One of the most compelling advantages of embolization is its minimally invasive nature. Unlike traditional surgery, embolization typically requires only a small incision and the insertion of a catheter, leading to less pain, lower risk of infection, and quicker recovery times. Patients often return to their normal activities much sooner than they would after surgery, with many procedures being performed on an outpatient basis.
The utility of embolization extends beyond these common applications, playing a critical role in less common but equally significant medical scenarios such as in the treatment of high-flow priapism, nosebleeds that are resistant to conventional treatments, and even in certain types of kidney and lung cancers. The procedure’s adaptability to various medical needs and its ability to provide targeted intervention with minimal downtime are what make embolization a valuable tool in modern medicine. Its ongoing evolution and integration into different medical fields underscore its potential to enhance patient outcomes across a myriad of health conditions.
Advantages of Embolization Over Other Treatments
Opting for embolization offers several advantages, including reduced recovery time and minimized surgical risks. Here, the benefits of this less invasive procedure are compared to traditional surgical interventions, providing patients with a clear understanding of their options.
Embolization stands out as a highly advantageous treatment option in various medical scenarios, primarily due to its minimally invasive nature, precision, and the substantial benefits it offers over more traditional surgical methods. This procedure has been revolutionary in treating conditions that are either difficult to manage surgically or where surgery poses significant risks. Here, we explore the key advantages of embolization compared to other treatment modalities, highlighting its efficiency, safety, and effectiveness.
Minimally Invasive Approach
One of the foremost benefits of embolization is its minimally invasive approach. Unlike conventional surgery, which often requires large incisions, embolization is typically performed through a small puncture in the skin. A catheter is then navigated through the blood vessels to the target area. This method significantly reduces the physical trauma to the patient, leading to less pain and quicker post-procedure recovery. The reduced invasiveness also minimizes the risk of infection and other complications associated with open surgeries.
Targeted Treatment
Embolization offers a high degree of precision, targeting problem areas directly without affecting surrounding tissues. This localized treatment approach is particularly beneficial in tumor management, where it is crucial to minimize damage to healthy tissue. By selectively blocking blood vessels that feed a tumor, embolization can effectively starve and shrink the tumor while preserving the functionality of the surrounding organs.
Reduced Hospital Stay and Recovery Time
Patients undergoing embolization typically experience shorter hospital stays and faster recovery times compared to those undergoing surgical interventions. Many embolization procedures are performed on an outpatient basis, allowing patients to return home the same day. The swift recovery not only enhances patient comfort but also reduces medical costs associated with prolonged hospital stays.
Lower Risk of Complications
The minimally invasive nature of embolization contributes to a lower risk of complications. Traditional surgeries, especially those involving vital organs or complex vascular structures, can lead to significant blood loss, infections, and long-term recovery issues. Embolization circumvents many of these risks by using body’s natural vascular pathways to deliver treatment directly to the affected area.
Versatility Across Multiple Conditions
Embolization’s versatility makes it suitable for treating a wide array of medical conditions. From reducing symptoms of benign prostatic hyperplasia (BPH) and managing uterine fibroids without the need for hysterectomy, to controlling life-threatening hemorrhages and reducing the size of vascular anomalies, embolization provides a robust solution across different fields of medicine.
Potentially Lower Overall Treatment Costs
While the initial procedure costs of embolization might be comparable to those of surgery, the overall treatment costs often turn out to be lower due to the reduced need for postoperative care, shorter hospital stays, and fewer complications that require additional treatment. This economic advantage is significant for both healthcare systems and patients, particularly in long-term management scenarios.
Improved Quality of Life
Patients who undergo embolization often report a higher quality of life post-treatment. The less disruptive nature of the procedure, coupled with reduced pain and quicker return to normal activities, contributes to overall patient satisfaction. Additionally, for conditions like uterine fibroids and BPH, where symptoms can severely affect daily life, embolization provides effective symptom relief with minimal impact on bodily integrity.
Aesthetic Benefits
For treatments involving visible areas of the body, such as facial vascular malformations, embolization avoids the scars associated with open surgery, offering superior aesthetic outcomes. This aspect is particularly important in pediatric and young adult patients, where long-term cosmetic outcomes can have profound psychological impacts.
In conclusion, embolization provides a multitude of advantages over traditional treatments, particularly in terms of invasiveness, recovery time, and targeted efficacy. These benefits make it a preferred choice for patients and doctors alike, especially in scenarios where reducing procedural risk and expediting recovery are paramount.
Post-Embolization Symptoms: What to Expect
Common Immediate Post-Procedure Symptoms
After embolization, patients might experience a range of symptoms, which are generally mild and manageable. This subsection will outline what is typically expected in the first few days following the procedure.
After undergoing an embolization procedure, patients can expect a variety of immediate post-procedure symptoms. While these symptoms are generally mild and manageable, being aware of what to expect can help patients prepare for the recovery process and identify any signs that may require further medical attention. Here’s a detailed look at the common symptoms that might occur shortly after embolization, providing insights into what is considered normal and what might be a cause for concern.
Post-Embolization Syndrome
One of the most frequently reported outcomes following embolization is post-embolization syndrome. This condition typically manifests as a constellation of symptoms including pain at the site of embolization, mild fever, nausea, and occasionally vomiting. These symptoms are thought to result from the body’s reaction to the foreign materials used to block the blood vessels and the subsequent death of tissue that was receiving blood from those vessels. Post-embolization syndrome is generally self-limiting and most often resolves within a few days.
Localized Pain and Discomfort
Localized pain at the catheter insertion site or in the area treated is common. Depending on the area embolized, patients might experience varying degrees of discomfort. For example, patients who undergo liver embolization might feel right upper quadrant pain, whereas uterine artery embolization can lead to pelvic discomfort. Over-the-counter pain relievers are usually sufficient to manage this pain, though sometimes prescription pain medication may be necessary.
Fatigue
Fatigue is another common symptom experienced by patients after embolization. This can be attributed to the body’s natural healing process and the emotional stress associated with undergoing a medical procedure. Rest is crucial, and patients are encouraged to take it easy for a few days post-procedure to allow their body to recover adequately.
Mild Fever
A mild fever can occur after embolization as part of the inflammatory response to the treatment. This should not be cause for alarm unless the fever is high (exceeding 101.5°F) or persists for more than a couple of days. Persistent or high fever could be a sign of infection or other complications requiring medical evaluation.
Nausea and Vomiting
These symptoms can occur, particularly if the embolization involves abdominal organs such as the liver or kidneys. Nausea and vomiting are usually temporary and can be managed with medications prescribed by the treating physician. If these symptoms persist, they may indicate an underlying complication that needs further investigation.
Changes in Urination or Bowel Movements
Depending on the location of the embolization, patients might notice changes in their urination patterns or bowel movements. For instance, those undergoing prostate or uterine artery embolization may experience temporary changes in urinary frequency or comfort, while liver embolization might affect bowel function. Typically, these symptoms are transient and resolve as the body adapts post-procedure.
Bruising and Minor Bleeding
Bruising at the catheter insertion site is common and usually harmless. Minor bleeding can also occur but should stop quickly with simple pressure. Extensive bleeding or bruising could be indicative of a more serious issue, such as a vascular injury, and should be assessed by a healthcare provider.
Emotional Reactions
It’s not uncommon for patients to experience emotional reactions such as anxiety or mood swings after a medical procedure. Support from healthcare providers, family, and friends can help manage these feelings effectively.
Recognizing these common immediate post-procedure symptoms helps patients to monitor their recovery and differentiate between normal healing processes and potential signs of complications. Maintaining open communication with healthcare providers during this time is crucial to ensure that any concerning symptoms are addressed promptly, ensuring a smooth and safe recovery period.
When to Be Concerned About Symptoms
Not all symptoms are benign. This part of the discussion focuses on differentiating between normal post-procedure experiences and signs that may indicate complications, such as excessive bleeding.
After embolization, while many symptoms are expected and part of the normal healing process, certain signs may indicate complications that necessitate immediate medical attention. Knowing when symptoms deviate from the norm is crucial for ensuring patient safety and the effectiveness of the treatment. Here, we discuss various symptoms that should raise concern and prompt patients or caregivers to seek professional medical help.
Severe or Worsening Pain
Although some degree of pain is normal after embolization, if the pain is severe, worsens over time, or becomes unmanageable with prescribed pain medications, it may be a sign of an underlying complication such as an infection, tissue damage, or a reaction to the embolic material. Severe pain that does not subside with conventional pain management strategies should be evaluated by a healthcare provider immediately.
High or Persistent Fever
While a mild fever following embolization can be a normal part of the body’s inflammatory response to the procedure, a high fever (over 101.5°F or 38.6°C) or a fever that persists for more than 48 hours could indicate an infection. Infections could be at the catheter insertion site or internally, related to the area of treatment. Immediate medical evaluation is necessary to rule out conditions such as sepsis, which can be life-threatening if not treated promptly.
Significant Swelling or Redness at the Catheter Site
Some swelling or redness at the catheter insertion site is typical. However, if the area becomes excessively swollen, red, feels hot to the touch, or shows signs of pus or unusual discharge, these could be signs of an infection or a reaction to the catheter itself. Such symptoms warrant a consultation with a healthcare professional to prevent further complications.
Changes in Mental Status
Changes in alertness, confusion, or extreme fatigue can be alarming and might indicate that the embolization has caused an unexpected effect, such as a stroke or a significant drop in blood pressure. These symptoms require urgent medical attention to determine the cause and provide the necessary interventions.
Persistent Nausea or Vomiting
While nausea and vomiting can occur after embolization, particularly if the abdomen is involved, persistent symptoms could hinder recovery and pose a risk of dehydration. Additionally, these symptoms could suggest complications such as a reaction to anesthesia, medication, or damage to surrounding organs.
Unusual Heartbeat or Shortness of Breath
If you experience palpitations, an unusually slow or fast heartbeat, or difficulty breathing after embolization, these could be signs of a cardiac issue or a pulmonary embolism, especially if the embolization was near the lungs or heart. These are serious conditions that require immediate emergency care.
Excessive Bleeding
Any bleeding that doesn’t stop with simple first aid measures, or significant bruising around the site of the embolization, might indicate that the vascular puncture hasn’t sealed properly or that there is internal bleeding. This is particularly critical to monitor in patients taking anticoagulant medication.
Loss of Function or Sensation
If there is a noticeable decrease in function or sensation in any part of the body, especially related to the treated area, this might indicate that the embolization has affected blood flow to critical tissues or nerves. Such symptoms should be assessed without delay to prevent long-term damage.
Recognizing these signs and responding promptly by seeking medical evaluation can significantly influence the outcome and effectiveness of the embolization procedure. Early detection and treatment of complications not only ensure patient safety but also enhance the overall success of the recovery process.

Is Bleeding Normal After Embolization?
Understanding Post-Embolization Bleeding
Bleeding can occur after any medical procedure, but is it normal after embolization? This section explains the causes of bleeding specific to embolization, how common it is, and the physiological reasons behind it.
Understanding the nature of post-embolization bleeding is crucial for patients who undergo this medical procedure, as it helps differentiate between normal healing and potential complications that require medical attention. Embolization, which involves intentionally blocking blood vessels to treat various medical conditions, can sometimes lead to bleeding issues, either immediately following the procedure or as a delayed response. Here we delve into the causes, commonality, and implications of bleeding after embolization.
Causes of Post-Embolization Bleeding
Bleeding after embolization can result from several factors related to the nature of the procedure and the specific condition being treated:
- Vascular Access Site Complications: The most common cause of bleeding is related to the site where the catheter was inserted. Vascular punctures can lead to complications such as hematoma (a solid swelling of clotted blood within the tissues), pseudoaneurysm, or arteriovenous fistula, especially if the puncture does not close properly.
- Reaction to Embolic Materials: Occasionally, the materials used to block the blood vessels can cause irritation or inflammation in nearby tissues, leading to bleeding. This is more likely if the embolization affects areas with extensive vascular networks.
- Residual or Collateral Blood Flow: In some cases, blood may find alternative pathways around the blocked vessel, especially in highly vascularized organs like the liver or kidneys. This can lead to increased pressure in smaller vessels that were not originally targeted, potentially causing them to leak or rupture.
- Tissue Necrosis: The intentional blocking of blood vessels leads to decreased blood supply, causing tissue necrosis (death of tissue). As the necrotic tissue breaks down, it may sometimes bleed, especially if the area is large or involves significant organ tissue.
How Common Is Bleeding After Embolization?
The incidence of significant bleeding following embolization is relatively low but varies depending on the type of embolization performed and the underlying health of the patient. Most bleeding that occurs is minor and can be managed with minimal intervention. However, the risk increases with:
- The complexity of the embolization
- The size and function of the organ involved
- Underlying health conditions that affect blood clotting
- Use of anticoagulant or antiplatelet medications
Assessing the Risk and Impact of Bleeding
The clinical impact of post-embolization bleeding ranges from benign to life-threatening. Assessing the risk involves several factors:
- Patient-specific factors: Age, overall health, and the presence of comorbid conditions (such as diabetes or hypertension) can influence bleeding risks.
- Procedure-specific factors: The type of embolization, the size and location of the vessels targeted, and the experience of the medical team all play roles.
- Post-procedure care: Proper management after embolization, including monitoring and follow-up care, significantly affects the outcome.
Management of Post-Embolization Bleeding
Management strategies for bleeding after embolization include:
- Immediate Care: Monitoring vital signs and the insertion site for signs of bleeding, along with routine lab tests to check blood counts and clotting status.
- Medications: Adjusting or temporarily halting anticoagulant and antiplatelet therapies may be necessary depending on the severity and location of the bleeding.
- Interventional Procedures: In cases where bleeding is significant or does not resolve with conservative measures, additional interventional procedures may be required to re-embolize the bleeding vessel or to apply other hemostatic techniques.
When to Seek Medical Help
Patients should be instructed to seek immediate medical help if they experience any of the following after embolization:
- Uncontrolled bleeding from the catheter insertion site
- Severe pain or swelling at the procedure site
- Signs of shock such as pallor, cold clammy skin, rapid heartbeat, or confusion
- Any sudden worsening of symptoms
Understanding and managing post-embolization bleeding is an essential aspect of patient care. With proper pre-procedural planning, risk assessment, and post-procedural care, most patients can achieve successful outcomes with minimal complications.
Types of Bleeding Associated with Embolization
Differentiating between minor bleeding and potentially dangerous bleeding is crucial for post-operative care. Here, we classify the types of bleeding that might occur and the implications of each.
Bleeding associated with embolization can vary in type and severity, depending on the specific procedure, the area treated, and the patient’s overall health. Understanding these variations is critical for both healthcare providers and patients to ensure prompt and effective management of any complications that may arise. Here, we explore the common types of bleeding that can occur after an embolization procedure.
Local Bleeding at the Catheter Insertion Site
The most straightforward and frequently observed type of bleeding is local bleeding at the site where the catheter was introduced, typically in the groin or wrist. This bleeding is usually minor and can be controlled with manual pressure or a compression device. However, in some cases, if the vascular access site does not seal properly, more significant bleeding or the development of a hematoma (a localized collection of blood outside of blood vessels) might occur.
Intracranial Hemorrhage
In procedures involving the arteries of the brain, such as embolization of brain aneurysms or arteriovenous malformations, there is a risk of intracranial hemorrhage. This type of bleeding can be extremely serious and requires immediate medical intervention. Symptoms may include sudden headache, nausea, vomiting, altered consciousness, and neurological deficits depending on the area of the brain affected.
Intra-abdominal Bleeding
Embolization procedures that target abdominal organs, like the liver, kidneys, or spleen, can sometimes lead to intra-abdominal bleeding. This might be due to the non-target embolization of adjacent tissues or the rupture of a blood vessel weakened by the procedure. Intra-abdominal bleeding can be challenging to detect early as it may not produce obvious symptoms until significant bleeding has occurred, potentially leading to signs of anemia or hypovolemic shock.
Retroperitoneal Hemorrhage
Retroperitoneal hemorrhage is a rare but potentially life-threatening complication, particularly in embolizations that involve large vessels within the retroperitoneal space (the area behind the abdominal cavity). Symptoms might include severe back pain, abdominal pain, a drop in blood pressure, and signs of internal bleeding.
Post-Embolization Syndrome Leading to Bleeding
Though not a direct cause of bleeding, post-embolization syndrome, which involves pain, fever, nausea, and sometimes vomiting, can exacerbate minor bleeding issues. For instance, severe vomiting might increase abdominal pressure and stress on treated vessels, potentially leading to bleeding complications.
Secondary Bleeding Due to Tissue Necrosis
In cases where embolization leads to significant tissue necrosis (tissue death due to lack of blood supply), secondary bleeding can occur as the necrotic tissue breaks down and sloughs away. This is particularly relevant in larger tumors or large areas of arteriovenous malformations that have been treated, where the loss of structural integrity in the tissue can lead to bleeding.
Managing Bleeding After Embolization
Immediate Steps to Take If Bleeding Occurs
If bleeding is noticed after embolization, there are specific steps that should be taken. This subsection provides a practical guide for patients to follow, helping them manage minor bleeding at home and recognizing when professional medical assistance is needed.
Long-Term Care and Monitoring
Beyond the immediate response, long-term care and monitoring are essential to ensure a safe recovery. This section discusses follow-up appointments, lifestyle adjustments, and other precautions that patients should consider.
Management strategies must be tailored to the type of bleeding encountered:
- Local and minor bleeding: Typically managed conservatively with pressure and monitoring.
- Significant internal bleeding: May require re-intervention, such as surgical exploration or a repeat embolization to address the bleeding source.
- Intracranial and retroperitoneal hemorrhages: Often demand immediate surgical intervention or intensive medical management in an emergency setting.
Prompt recognition and appropriate response to the type of bleeding are essential for optimizing patient outcomes after embolization. Education on potential symptoms and when to seek medical help should be an integral part of pre-procedural counseling for all patients undergoing embolization.
When to Seek Medical Help
Signs That Indicate a Medical Emergency
Not all complications can be handled at home. Identifying the signs of a serious issue post-embolization is a critical aspect of recovery. Here, we outline symptoms that necessitate urgent medical attention.
Consulting with Healthcare Providers
Maintaining open communication with healthcare providers post-procedure is vital. This part emphasizes the importance of regular check-ups and what to discuss during these consultations.
Patient Experiences with Embolization
Real-Life Stories of Post-Embolization Recovery
Sharing experiences from patients who have undergone embolization can provide comfort and practical insights to those facing the procedure. This section includes testimonials highlighting both the challenges and successes of recovery.
Statistics on Recovery Outcomes
To give readers a broader perspective, this subsection provides statistical data on recovery rates, complications, and overall success of embolization procedures.
Conclusion
Understanding the normalcy and risks of bleeding after embolization is essential for anyone undergoing this procedure. While minor bleeding can be a common part of the recovery process, significant bleeding requires immediate medical attention. By being informed about what to expect and when to seek help, patients can effectively manage their recovery and minimize potential complications.
FAQs
- What are the immediate steps I should take if I notice bleeding after embolization?
- How long does it typically take to recover from an embolization procedure?
- What are the signs of infection or complications I should watch for after embolization?
- Can embolization be performed more than once if needed?
- Are there any lifestyle changes I should consider to aid in my recovery?
- What are the long-term effects of embolization on my health?
Bleeding after embolization, while concerning, is often manageable and may be expected depending on the specifics of the procedure and patient condition. Being prepared and knowledgeable about what to expect can significantly ease the recovery process, making it smoother and more comfortable for the patient.
Our Doctors
Dedicated IR Center for Vascular Problems in Madhya Pradesh
DR. SHAILESH GUPTA
MD, PDCC (INTERVENTIONAL RADIOLOGY) Consultant & Co-Director CVIC (Center Of Vascular & Interventional Care)
DR. ALOK KUMAR UDIYA
MD Radiology, PDCC (Neuro intervention Radiology), PDCC ( HPB Intervention Radiology) FINR (Switzerland) & EBIR
Endovascular Surgeon & Consultant Interventional Neuroradiologist at Care CHL Hospital, Indore Co-director CVIC( center for vascular and interventional care) https://interventionradiologyindore.com/
DR. NISHANT BHARGAVA
Consultant Intervention Radiologist
MD Radiology, PDCC ( Neuro intervention Radiology), FINR ( Fellowship in Neuro intervention Radiology)
Co-director CVIC(Center for Vascular and Interventional Care)
Contact Details
Phone no.
0731 4675670
+91 9827760073
Facebook
https://www.facebook.com/profile.php?id=100092538633553&mibextid=ZbWKwL
Instagram
https://instagram.com/cvic_center?igshid=ZGUzMzM3NWJiOQ==
Google My business
https://g.co/kgs/DrdV3T
YouTube
https://www.youtube.com/channel/UCP5TH5e4iQZkpDUgnLsgZhw
Pinterest
https://pin.it/5DzpX5Z
Twitter
https://x.com/cviccenter?t=01TclSrLFdu0K2re0Gs96w&s=08
LINKEDIN
https://www.linkedin.com/company/center-of-vascular-interventional-care/
Location
Bleeding After Embolization
Read More –
Vertebroplasty: What It Is, Purpose, Procedure & Side Effects – https://cvicvascular.com/vertebroplasty-what-it-is-purpose-procedure-side-effects/
Empowering Women: A Comprehensive Guide to Uterine Artery Embolization (UAE) – https://cvicvascular.com/uterine-artery-embolization-uae/
Placenta Previa: Symptoms, Causes & Treatments – https://cvicvascular.com/placenta-previa/