Peripheral Artery Disease (PAD) is a common circulatory condition that often goes unnoticed due to its similarity to regular muscle cramps. Recognizing how PAD symptoms differ from regular muscle cramps is crucial for early detection and treatment. While muscle cramps can result from various causes like dehydration or muscle strain, PAD symptoms signal a more serious issue linked to poor blood flow and potential cardiovascular complications.
In this blog, we’ll break down the major differences between PAD symptoms and regular muscle cramps to help you understand when to seek medical advice. Spotting these differences can make a significant impact on your health journey.
What Are PAD Symptoms?
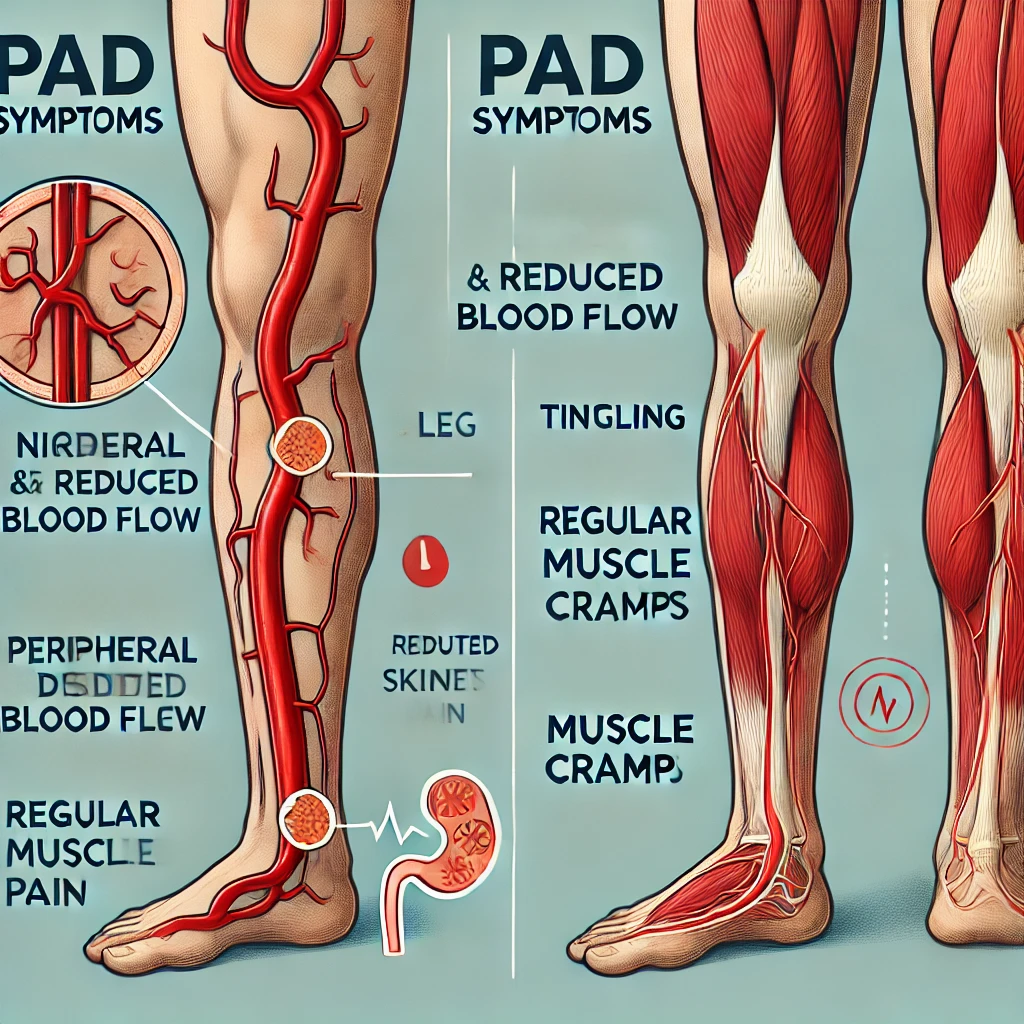
Peripheral Artery Disease, commonly referred to as PAD, results from narrowed arteries that reduce blood flow to the limbs. Most commonly, it affects the legs, which can experience pain, fatigue, or discomfort when walking or engaging in physical activities.
PAD symptoms often include:
- Leg pain, especially during exercise or walking, which lessens after resting
- Numbness or weakness in the legs
- Coldness in the lower leg or foot, especially when compared to the other side
- Poor wound healing in the affected areas
- Changes in skin color and texture
Regular Muscle Cramps
On the other hand, muscle cramps are generally caused by muscle fatigue, dehydration, or overuse. They are temporary, often harmless, and can occur in various muscle groups, including the legs, arms, and hands. Regular muscle cramps can also be linked to low levels of certain minerals, such as potassium or magnesium, and typically subside within minutes.
Also Read: What Conditions Does an Endovascular Surgeon Treat?
Key Differences Between PAD Symptoms and Muscle Cramps
1. Cause of the Pain
PAD Symptoms
PAD symptoms stem from a restricted blood flow due to the narrowing of arteries, particularly in the legs. This reduction in blood flow causes pain during activities as the muscles are deprived of adequate oxygen and nutrients. PAD pain is a sign of underlying vascular issues that require medical attention.
Regular Muscle Cramps
Regular muscle cramps, however, are commonly due to temporary muscle fatigue or dehydration. For example, athletes or people who exercise intensely may experience cramps due to overuse or electrolyte imbalances. They typically resolve quickly once the muscle relaxes or is stretched.
2. When and How the Pain Occurs
PAD Symptoms
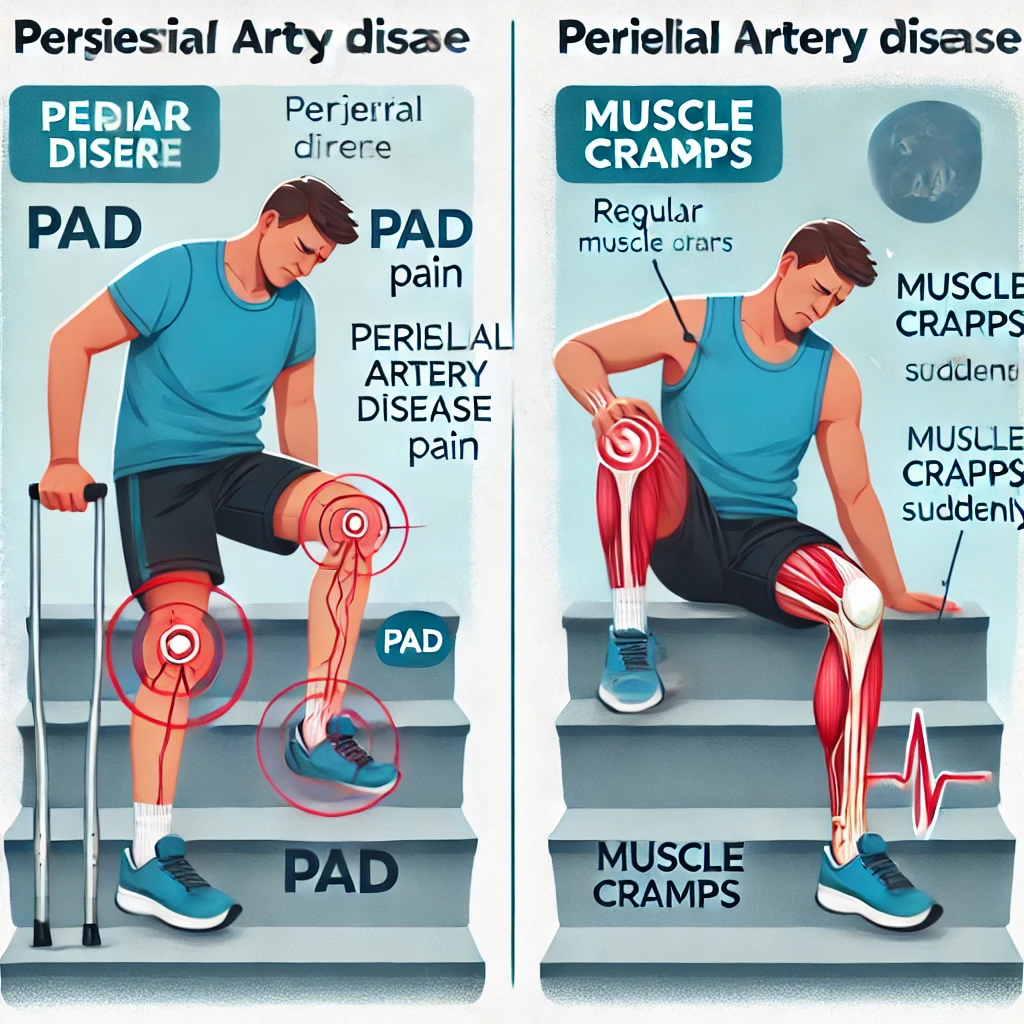
PAD symptoms often appear during physical activity, especially walking or climbing stairs, and subside with rest. Known as “claudication,” this pain can feel like an intense cramp or ache that comes on consistently with physical exertion.
Regular Muscle Cramps
In contrast, muscle cramps can happen anytime and are often abrupt and unpredictable. A person may experience a cramp while sleeping, sitting, or stretching. Unlike PAD pain, muscle cramps are not directly linked to blood flow issues but rather to sudden muscle contraction.
3. Duration and Frequency of Pain
PAD Symptoms
PAD symptoms are persistent and may worsen over time. As the condition advances, the frequency and intensity of the pain increase. In severe cases, pain may occur even at rest, indicating a critical restriction of blood flow. This type of pain is unlikely to resolve quickly without medical intervention.
Regular Muscle Cramps
Muscle cramps are usually brief, lasting only a few seconds to a couple of minutes. While uncomfortable, they generally resolve on their own or with gentle stretching. The frequency of muscle cramps can vary based on activity levels, but they do not typically escalate in severity over time.
Also Read: What Are the Benefits of Interventional Radiology?
4. Areas Affected by the Pain
PAD Symptoms
PAD primarily affects the lower limbs, specifically the calf muscles, thigh, or buttocks. This localized pain pattern is due to blocked arteries in the legs. Additionally, PAD symptoms are associated with other issues in the affected area, such as skin color changes or wounds that heal slowly.
Regular Muscle Cramps
Muscle cramps can occur in various muscle groups and are not limited to the lower limbs. While common in the legs, they can affect any voluntary muscle, including those in the arms, abdomen, or back.
5. Accompanying Symptoms
PAD Symptoms
In addition to leg pain, PAD symptoms often include numbness, weakness, and a feeling of heaviness in the legs. Physical signs like a cold foot or toes, reduced hair growth on the legs, and brittle toenails can also be indicators of PAD. These symptoms suggest chronic circulatory issues.
Regular Muscle Cramps
Muscle cramps, on the other hand, are rarely accompanied by other symptoms. They often come and go quickly, leaving little to no lasting effect on the muscle. Although painful, muscle cramps generally do not cause numbness, weakness, or visible changes in the skin.
6. Treatment and Prevention Approaches
PAD Symptoms
Treating PAD requires medical intervention, typically involving lifestyle changes, medication, or even surgery in severe cases. Smoking cessation, exercise, and a balanced diet are essential for managing PAD symptoms. Early detection is key to preventing the progression of the disease and avoiding serious complications.
Regular Muscle Cramps
Regular muscle cramps can often be prevented or managed with hydration, stretching, and electrolyte balance. Over-the-counter pain relief may help with occasional cramps, but they typically do not require long-term treatment.
Understanding the Risks: Why PAD Symptoms Should Not Be Ignored
Unlike muscle cramps, PAD symptoms indicate a serious underlying issue. PAD is a progressive disease, and if left untreated, it can lead to severe complications, including critical limb ischemia, ulcers, and even amputation in advanced cases. PAD also increases the risk of heart attack and stroke due to its link with atherosclerosis, the hardening and narrowing of the arteries throughout the body.
Also Read: How Can I Prevent Diabetic Foot Problems? 10 Essential Tips for Healthy Feet
Frequently Asked Questions
What is the main difference between PAD symptoms and regular muscle cramps?
PAD symptoms are due to restricted blood flow in the arteries, leading to pain that usually occurs during activity and subsides with rest. Muscle cramps, however, are often caused by dehydration or muscle fatigue and occur unpredictably.
How long do PAD symptoms last?
PAD symptoms tend to persist and can worsen over time, especially if left untreated. In severe cases, pain may be present even at rest.
Can PAD symptoms be treated with home remedies?
While lifestyle changes can help manage PAD symptoms, medical intervention is often required for effective treatment. Regular check-ups, medication, or procedures may be necessary to improve blood flow.
Why do muscle cramps occur at night?
Muscle cramps can happen at night due to factors like dehydration, electrolyte imbalance, or muscle overuse. They are generally harmless and resolve quickly.
How can I differentiate between PAD and muscle cramp pain?
PAD pain often occurs during activity and eases with rest, while muscle cramps can happen anytime. PAD pain also tends to be more persistent and can be accompanied by numbness, coldness, or skin changes.
Is PAD a reversible condition?
PAD is a chronic condition, but its symptoms can be managed with lifestyle changes, medication, and, in some cases, surgical procedures to improve blood flow. Early detection plays a significant role in managing PAD effectively.
Conclusion
Understanding the differences between PAD symptoms and regular muscle cramps can be crucial for early detection of Peripheral Artery Disease. While muscle cramps are usually a benign condition with minimal health risks, it’s symptoms indicate potential circulatory issues that need medical evaluation. Noticing these distinctions in pain, location, and accompanying symptoms can lead to timely intervention, reducing the risk of complications and improving overall health.
Taking proactive steps to consult a healthcare provider if you experience consistent pain during activities can make a significant difference in managing PAD and maintaining a healthy lifestyle. By learning the signs, you’re already taking the first step toward better vascular health.