Tumor embolization, a pivotal treatment in the realm of oncology, offers a beacon of hope for many patients grappling with various types of tumors. This minimally invasive procedure involves blocking the blood supply to a tumor, thereby starving it of the nutrients it needs to grow. The success rate of this technique not only shines a light on its effectiveness but also underscores the advancements in medical technology and technique. This article delves deep into understanding the intricacies of tumor embolization, its success rates across different tumors, and the factors that influence these outcomes.
Understanding Tumor Embolization
The Mechanics of Tumor Embolization
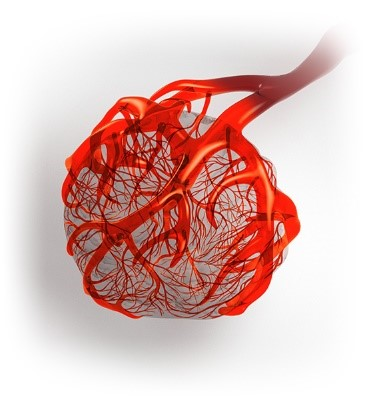
Tumor embolization works by introducing substances that obstruct the tumor’s blood vessels. This blockage can be achieved using various materials, including small particles, coils, or other agents, administered through a catheter placed directly into the blood supply of the tumor. The procedure not only restricts tumor growth but also minimizes blood loss during surgery, making subsequent treatments more manageable.
Types of Tumors Treated with Embolization
Tumor embolization stands as a cornerstone in the minimally invasive treatment of various tumor types, playing a crucial role in oncology for patients whose conditions either cannot be managed through conventional surgery or require additional intervention to control tumor growth. This specialized procedure is employed across a range of tumors, predominantly benefiting patients by targeting the tumor’s blood supply, thus restricting its ability to thrive and spread. Here, we explore the various types of tumors that are commonly treated with embolization, shedding light on the versatility and effectiveness of this technique.
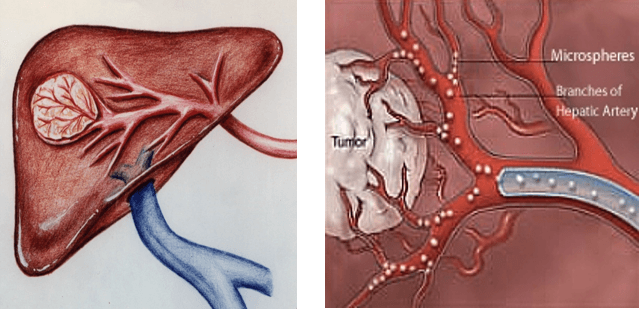
Liver Tumors: Primary and Metastatic
Liver tumors are perhaps the most frequent candidates for embolization. This includes both primary liver cancers, such as hepatocellular carcinoma (HCC), and liver metastases from other cancer origins like colorectal cancer. Embolization is particularly beneficial for patients who may not be suitable for surgery due to the location or number of tumors, or due to underlying conditions such as cirrhosis which may complicate traditional surgical interventions.
- Hepatocellular Carcinoma (HCC): As the most common type of primary liver cancer, HCC is a prime target for embolization. The procedure can be curative or palliative, depending on the stage of the cancer and overall liver function.
- Metastatic Liver Cancer: Tumors that have spread to the liver from other areas of the body can also be treated with embolization. This is especially common with metastases from colorectal cancer, neuroendocrine tumors, and breast cancer.
Kidney Tumors
Embolization is also used in the management of kidney tumors, particularly in cases where surgery poses too high a risk, or when the patient’s other health issues contraindicate surgical intervention. Renal cell carcinoma (RCC), the most common type of kidney cancer, often sees benefit from embolization, either as a pre-surgical measure to reduce blood loss or as a standalone treatment to manage symptoms and tumor progression.
Uterine Fibroids
While technically benign, uterine fibroids can cause significant symptoms such as heavy menstrual bleeding, pain, and pressure on other pelvic organs. Uterine fibroid embolization (UFE) is a highly effective treatment that blocks the arteries supplying blood to the fibroids, causing them to shrink and symptoms to lessen. This procedure offers an important non-surgical option for women who wish to avoid hysterectomy.
Neuroendocrine Tumors
Neuroendocrine tumors (NETs), which can occur in various locations including the pancreas and gastrointestinal tract, are another type of tumor treated with embolization. These tumors often produce hormones that can cause severe symptoms. Embolization helps to reduce hormone production and tumor growth, providing symptomatic relief and enhancing quality of life.
Bone Tumors
Embolization can be used to treat painful, aggressive benign bone tumors such as giant cell tumors as well as some malignant bone cancers to reduce tumor size and alleviate symptoms. It is often used as a preoperative measure to decrease the risk of bleeding during surgery.
Meningiomas and Other Brain Tumors
In certain cases, embolization is utilized to treat brain tumors like meningiomas, particularly those that are difficult to access surgically. By reducing the tumor’s blood supply, embolization can decrease the tumor’s size and lower the risks associated with surgical removal.
The decision to use embolization as a treatment approach depends on a multitude of factors, including the type of tumor, its location, the patient’s overall health, and specific medical circumstances. As technology and techniques continue to evolve, the scope of tumors treatable with embolization is likely to expand, offering new hope and possibilities to patients facing complex oncological challenges. This reflects not only the adaptability of embolization as a treatment modality but also its crucial role in the multidisciplinary approach to cancer care.
Evaluating the Success Rates of Tumor Embolization
Success Rate Variability by Tumor Type
The success of tumor embolization largely depends on the type of tumor being treated. For instance, in the treatment of liver tumors such as hepatocellular carcinoma (HCC), embolization can achieve success rates as high as 70-90% in preventing tumor progression. Kidney and neuroendocrine tumors also show favorable responses, with significant percentages achieving stability or reduction in tumor size.
Factors Influencing Success Rates
Tumor embolization is a sophisticated medical procedure that plays a significant role in the management of various tumors by obstructing their blood supply, ultimately aiming to reduce tumor size or alleviate symptoms. While the procedure offers a promising outlook, its success rate can be significantly influenced by several factors. Understanding these factors is crucial for both medical practitioners and patients to set realistic expectations and optimize treatment outcomes. Here, we explore the primary elements that affect the success rates of tumor embolization.
Tumor Characteristics
Type and Histology of the Tumor
Different types of tumors respond differently to embolization. Tumors that are highly vascular, such as hepatocellular carcinoma (HCC) or renal cell carcinoma (RCC), generally respond better to embolization because the procedure targets the blood vessels feeding the tumor. The histological characteristics of the tumor can also impact how effectively the embolic agents can induce necrosis or reduce tumor size.
Size and Location of the Tumor
The size and location of the tumor significantly influence the success of embolization. Smaller tumors are often more effectively treated because embolic agents can more readily block their limited blood supply. Tumors located in areas with complex vascular architecture may pose challenges in selectively targeting the necessary blood vessels, potentially reducing the procedure’s efficacy.
Technical Factors
Choice and Delivery of Embolic Agents
The type of embolic material used and its delivery are pivotal to the success of embolization. Agents range from microspheres and beads to liquid agents that can conform to the shape of the blood vessels. The choice depends on the desired level of occlusion, the type of tumor, and the specific characteristics of the tumor’s blood supply. Precise delivery of these agents, often guided by advanced imaging techniques, is crucial to ensure that the embolization effectively targets the tumor without affecting surrounding tissues.
Interventional Radiologist’s Expertise
The skill and experience of the interventional radiologist play a critical role in the success of tumor embolization. Expertise in navigating the vascular system, accurately positioning the catheter, and effectively deploying embolic agents are essential for a successful outcome. Experienced specialists are likely to achieve higher success rates due to their ability to manage complex cases and make real-time decisions during the procedure.
Patient Factors
Overall Health and Comorbidities
A patient’s general health, including the presence of other medical conditions, can influence the outcomes of tumor embolization. Patients in good overall health with fewer comorbidities tend to recover faster and experience fewer complications. Conversely, conditions such as poor liver or kidney function can complicate the procedure and recovery process, potentially affecting its success.
Tumor’s Response to Previous Treatments
The tumor’s history with other treatments can also affect embolization outcomes. Tumors that have shown resistance to other forms of treatment, such as chemotherapy or radiation, might exhibit a similar resistance to embolization. Conversely, tumors that have responded well to prior treatments may also show positive outcomes with embolization.
Post-Procedure Care
Follow-Up and Monitoring
Successful embolization does not end with the procedure itself; meticulous post-procedure follow-up is vital. Monitoring for potential complications, assessing the tumor’s response through imaging, and managing any symptoms post-embolization are integral to the overall success. Regular follow-ups help in timely detecting any recurrence or growth of the tumor and planning further treatment if necessary.
Patient’s Compliance with Follow-Up Care
Patient adherence to follow-up schedules and care recommendations significantly impacts the success of the treatment. Patients who actively engage in their follow-up care and adhere to medical advice regarding lifestyle changes and medication are more likely to see positive outcomes from embolization.
The success of tumor embolization is multifaceted, influenced by a blend of tumor-specific, technical, and patient-related factors. A thorough understanding of these elements can help healthcare providers better plan and execute embolization procedures, tailor treatments to individual patient needs, and ultimately enhance the success rates and quality of life for those undergoing this innovative treatment.
The Patient Journey Through Tumor Embolization
Pre-Procedure Considerations
Tumor embolization is a strategic intervention in oncology, used to treat various tumors by restricting their blood supply. This minimally invasive procedure requires careful planning and consideration to ensure safety and maximize treatment efficacy. Pre-procedure considerations are crucial steps in the treatment planning process, involving comprehensive assessments and preparations. These steps not only prepare the patient physically but also equip the medical team with vital information to execute the procedure effectively. Here, we explore the essential pre-procedure considerations for tumor embolization.
Medical Evaluation and Consultation
Comprehensive Patient History
A thorough review of the patient’s medical history is fundamental. This includes understanding past and current medical conditions, previous treatments or surgeries, and any allergies or adverse reactions to medications or contrast agents. A detailed history helps in anticipating potential complications and tailoring the procedure to the patient’s specific health needs.
Discussion of Treatment Objectives
Clear communication between the patient and the healthcare provider regarding the goals of the embolization is essential. This discussion should cover what the procedure entails, the expected outcomes, and the realistic goals of treatment, whether it’s palliative or curative. Understanding the patient’s expectations and concerns is also vital to provide support and ensure they are well-informed.
Diagnostic Imaging
Radiological Assessments
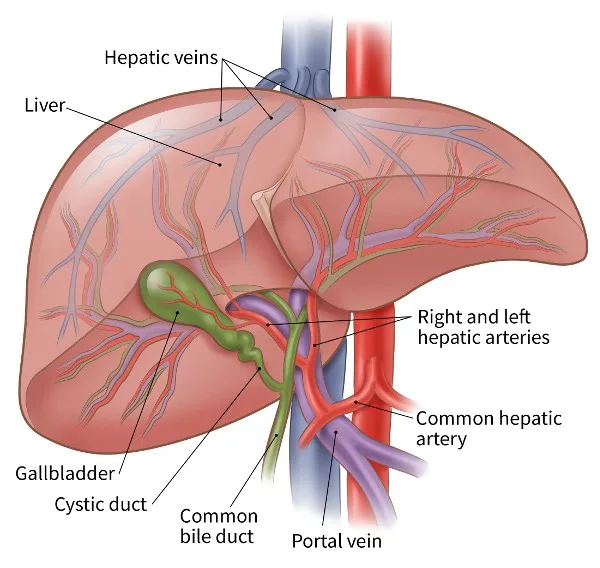
Imaging studies play a pivotal role in the pre-procedure planning of tumor embolization. Techniques such as computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound help in mapping the tumor’s size, location, and vascularity. These imaging studies are crucial for detailed planning of the embolization approach, including the selection of the best route for catheter placement and the choice of embolic materials.
Angiography
Pre-procedural angiography is often conducted to provide a detailed view of the vascular anatomy and the blood supply to the tumor. This procedure can pinpoint the specific arteries feeding the tumor and assess the collateral blood flow, which is crucial for planning the embolic strategy to minimize damage to surrounding tissues.
Laboratory Tests
Blood Tests
Comprehensive blood tests are required to evaluate the patient’s overall health status. Key parameters include liver and kidney function tests, coagulation profiles, and complete blood counts. These tests are necessary to ensure the patient is fit for the procedure and to identify any potential issues that could complicate the embolization, such as clotting disorders or impaired organ functions.
Medication Review and Management
Adjusting Current Medications
Patients may need to adjust their current medications prior to embolization. For example, medications that affect blood clotting, such as anticoagulants or non-steroidal anti-inflammatory drugs (NSAIDs), may need to be temporarily discontinued to reduce the risk of bleeding.
Prophylactic Antibiotics
In some cases, prophylactic antibiotics may be administered before the procedure to prevent infection, especially if the embolization involves regions where bacterial contamination is a concern, such as the gastrointestinal tract.
Patient Preparation and Education
Fasting Before the Procedure
Patients are usually required to fast for several hours before the procedure to reduce the risk of aspiration and to prepare for potential sedation. Clear instructions about the fasting period and what is allowed or not allowed should be provided well in advance.
Education on Risks and Post-Procedure Care
Educating the patient about the potential risks, complications, and the typical post-procedure care is essential. This includes information on what to expect immediately after the procedure, potential signs of complications, and the recovery process. Well-informed patients are more likely to comply with post-procedure instructions and report any issues promptly, contributing to a successful outcome.
Ensuring thorough pre-procedure considerations for tumor embolization is vital for the safety and success of the treatment. These steps not only prepare the patient but also enable the medical team to tailor the procedure according to the specific clinical nuances of each case. Such diligent preparation is instrumental in enhancing the efficacy of tumor embolization and optimizing patient outcomes.
The Embolization Procedure: Step by Step
- Preparation: Patients may be given medications to help with anxiety and pain.
- Catheter Insertion: A catheter is inserted into an artery and navigated to the feeding artery of the tumor.
- Delivery of Embolic Agents: Agents are injected through the catheter to block the blood vessels.
- Post-Procedure Monitoring: After the procedure, patients are monitored for any adverse reactions and effectiveness of the treatment.
Post-Procedure Recovery and Follow-up
Recovery times can vary, but patients usually resume normal activities within a few days. Follow-up care is crucial to monitor the tumor’s response to the embolization and to detect any recurrence early.
Advancements and Innovations in Tumor Embolization
Recent technological advancements have significantly improved the precision and outcomes of tumor embolization. Innovations such as drug-eluting beads and more targeted delivery systems enhance the procedure’s effectiveness while minimizing side effects.
Frequently Asked Questions
What are the main risks associated with tumor embolization?
The risks include infection, bleeding, and unintended blockage of blood flow to healthy tissues, although these are relatively rare with advanced techniques.
How long does it take to see results from tumor embolization?
Results can vary; some patients might notice improvements in symptoms within a few weeks, while for others, it might take longer to assess the full impact of the treatment.
Can tumor embolization be repeated if the tumor regrows?
Yes, embolization can be repeated in some cases, depending on the patient’s overall health and the specific characteristics of the tumor.
Is tumor embolization covered by insurance?
Most insurance plans cover tumor embolization, but coverage can vary based on the type of tumor and the specific policy.
What are the alternatives to tumor embolization?
Alternatives may include traditional surgery, radiation therapy, and newer forms of treatment like targeted therapy and immunotherapy, depending on the tumor type.
Conclusion
Tumor embolization represents a significant advancement in the treatment of certain tumors, offering hope and improved quality of life to many patients. Its success rates, while varying, generally reflect a positive trend thanks to ongoing innovations and tailored approaches. As research continues and technology advances, tumor embolization is likely to play an increasingly vital role in cancer treatment strategies.
Our Doctors
Dedicated IR Center for Vascular Problems in Madhya Pradesh
DR. SHAILESH GUPTA
MD, PDCC (INTERVENTIONAL RADIOLOGY) Consultant & Co-Director CVIC (Center Of Vascular & Interventional Care)
DR. ALOK KUMAR UDIYA
MD Radiology, PDCC (Neurointervention Radiology), PDCC ( HPB Intervention Radiology) FINR (Switzerland) & EBIR
Endovascular Surgeon & Consultant Interventional Neuroradiologist at Care CHL Hospital, Indore Co-director CVIC( center for vascular and interventional care)https://interventionradiologyindore.com/
DR. NISHANT BHARGAVA
Consultant Intervention Radiologist
MD Radiology, PDCC ( Neurointervention Radiology), FINR ( Fellowship in Neurointervention Radiology)
Co-director CVIC(Center for Vascular and Interventional Care)
Contact Details
Phone no.
0731 4675670
+91 9827760073
Facebook
https://www.facebook.com/profile.php?id=100092538633553&mibextid=ZbWKwL
Instagram
https://instagram.com/cvic_center?igshid=ZGUzMzM3NWJiOQ==
Google My business
https://g.co/kgs/DrdV3T
YouTube
https://www.youtube.com/channel/UCP5TH5e4iQZkpDUgnLsgZhw
Pinterest
https://pin.it/5DzpX5Z
Twitter
https://x.com/cviccenter?t=01TclSrLFdu0K2re0Gs96w&s=08
LINKEDIN
https://www.linkedin.com/company/center-of-vascular-interventional-care/
Location
Read More –
What is a PCN Procedure in Urology? – https://cvicvascular.com/what-is-a-pcn-procedure-in-urology/
How Do You Take Care of a Perma Cath? – https://cvicvascular.com/how-to-take-care-of-a-perma-cath/
How Long Does It Take to Remove a DJ Stent? – https://cvicvascular.com/how-long-does-it-take-to-remove-dj-stent/